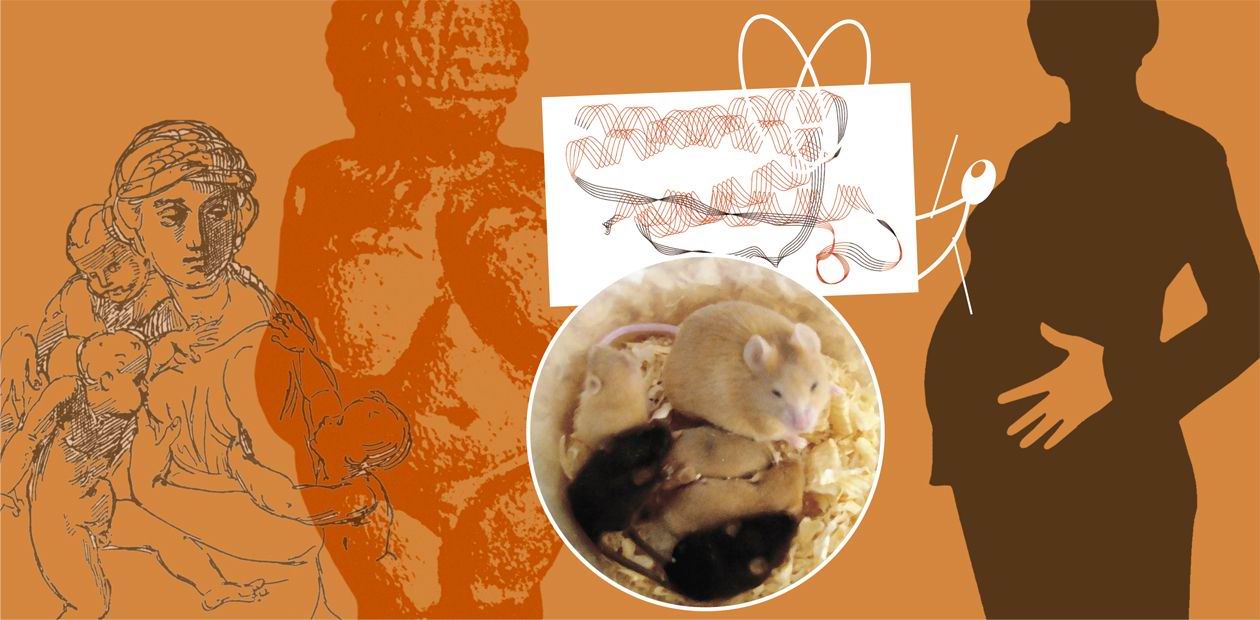
Pregnancy as a Remedy for Obesity
Obesity as a problem is a phenomenon peculiar only to a developed human society. Another problem — hunger —is characteristic of wild nature just as of the prehistoric human society. Hence, a healthy fatness at all times was an indicator of a physical and social prosperity. In modern society, this opinion has survived perhaps only towards children and pets. So, what is obesity — a bad habit or a disease? Why does it require so much effort to lose excess kilos? Is it feasible to correct the overweight? The research with model objects — mice with genetically determined obesity — throws light on this modern “plague” of the replete humankind...
Today, few people in industrially developed countries are not troubled with the problem of overweight: just take the Unites States — they even speak about the epidemic of obesity. Obesity is hazardous not only because the carriers of excess kilos are far in their appearance from ephemeral creatures — an ideal for the modern fashion — and even not because they have to spend much more money and time for purchasing footwear and clothes. The main thing is that obesity inevitably entails a chain of diseases. Those suffering from obesity encounter an increased risk to die of many diseases, such as diabetes, hypertension, occlusion of heart blood vessels, stroke, various gall-bladder and liver diseases, cancer, and even respiratory arrest in their sleep…
For many years scientists and physicians have tried to find ways to prevent obesity development. It is well known that the fat laid in store is simply an unnecessary, unspent energy coming with food. As early as 10 years ago, they believed that obesity is the result of laziness and overeating and is easily treatable: just eat less and move more. The cruelest diets based on calculation of the calories consumed helped most people to reach a temporary weight loss; but the weight steadily restored once the restictions were removed.
However, the year 1994 brought two events that altered radically our attitude to the treatment of obesity. First, the hormone of fatty tissue — leptin — was discovered. Second, the melanocortin system of the brain, wherethrough this hormone regulates the fat metabolism, was described.
Leptin: the controller of fat reserves
As appeared, fat is not just a “pillow” that blemishes a lovely figure, but also an endocrine organ producing a protein hormone. However, if an organ is capable of secreting hormones into the blood, then it is capable of influencing the functions of other organs and physiological systems. Thus, this is leptin due to which the fat as if “struggles” for its existence (Cone et al., 2001).
The level of leptin excreted by fatty cells elevates with an increase in the size of these cells. At high concentrations, this hormone prevents further obesity development by suppressing appetite and increasing energy expenditure. However, a drastic decrease in the fat percent in the body (for example, by liposuction or a diet), also decreases the level of leptin and, consequently, removes its inhibiting effect on appetite. Therefore, a drastic loss of weight also implies a drastic drop in the leptin level, which causes an increased appetite. In other words, leptin prevents both people with a normal weight from developing further obesity and stout persons from losing weight. So, why are people yet able to gain this much weight? Merely because when the level of leptin in the blood becomes very high, these people become insensitive to this hormone. But it is another tale.
Who will give the supper to an enemy?*
Thus, leptin is able to affect appetite, i. e., a complex physiological feature, which is called the food behavior. Similar to all forms of behavior, it is regulated by various regions of the brain and, first and foremost, by hypothalamus. At the end of 1990s it was found that leptin acts on appetite via the melanocortin system (MC system) of the hypothalamus.
Let us start with a brief digression into the family of specific melanocortin hormones. This group covers melanocyte-stimulating hormones (MSH), including those regulating pigment production, and adrenocorticotropic hormone (ACTH) regulating the function of the adrenal glands. All these hormones have a common precursor molecule, similar amino acid sequences in their structure, and are recognized by receptors belonging to the same family.
Initially, when these hormones were found to be closely related, noone could surmise that this system also had its local representation in the hypothalamus, which is responsible for the regulation of energy input and consumption. This so-called MC system of hypothalamus is the target of leptin action. To understand the mechanism of its action, we need a brief acquaintance with the function of the melanocortin system.
Neurons of the hypothalamus are capable of producing one of the melanocyte-stimulating hormones (α-MSH), activating in it specific melanocortin receptors, which, in turn, results in appetite suppression. Therefore, the hypothalamic α-MSH is ascribed to anorectic factors — the factors that reduce the desire to eat. But for the existence of orectic factors, that increase appetite along with anorectic ones, there would be no problem of obesity. Indeed, there would arise a more terrible problem — to die of hunger with plenty of food.
Mother Nature is wise: along with anorectic α-MSH, other neurons of the hypothalamus produce orectic peptide (agouti-like protein, ALP). ALP is able to block α-MSH binding to its receptors, thereby increasing appetite. The ratio between the production of anorectic and orectic factors — α-MSH and ALP — in the hypothalamus determines how easy you can refuse your dinner when following the advice of dietitians.
Leptin is the “conductor” of this ensemble: it stimulates α-MSH and inhibits ALP synthesis, which brings about a decrease in appetite. A decrease in the leptin level in the blood induces the opposite effect — appetite increases. Under natural conditions, wild species never encounter the problem of obesity: the ability of leptin to adjust appetite to the available fat reserves is an efficient mechanism of adaptation to the hunger conditions. Food deficiency unfolds the following chain of events: fat percent decreases, leptin level drops, and appetite increases concurrently with the consumption rate of the available energy reserves.
Genetic obesity
Returning to the problem of obesity, it is once again necessary to specify what particular changes in the hypothalamic MC system must result in the appetite increase and weight gain. Appetite will be stimulated in one of the following cases: (1) a decrease in the production of α-MSH; (2) a decrease in the number of melanocortin receptors or their ability of binding α-MSH; or (3) an increase in the production of ALP or any other blocker of melanocortin receptors.
The correctness of this inference is confirmed by that various strains of laboratory mice with artificial mutations impairing the function of the genes encoding the mentioned proteins and, respectively, their production, have been bred. All these mice suffer with the so-called melanocortin obesity. Apropos, mice entered upon our stage not at all accidentally. Luckily for us, the weight regulation system is similar in all mammals, including humans and mice, the latter being a convenient object for physiological studies.
As early as 10 years ago, they believed that obesity is the result of laziness and overeatingOne mouse strain, C57Bl/6J, stands alone, as the mutation causing obesity in this strain appeared spontaneously. It is a somewhat incentive reward for the scientists involved in the research into the mechanisms of MC obesity. As a matter of fact, this strain was long known by the mutations at Agouti locus, controlling the color of the mouse’s fur. Mice with the dominant mutation at this locus, Agouti yellow(Ay), have yellow fur, whereas individuals with the recessive mutation, nonagouti (a), are colored black. Reaching puberty, the yellow mice develop obesity and type 2 diabetes, which the black mice luckily escape.
Mutations in various components of the melanocortin system of the hypothalamus were detected in the majority of people suffering with obesityThe connection between the fur color and the tendency to obesity was a riddle for a long time — until Bultmann et al. (1991) demonstrated that the mutation Agouti yellow impaired the pattern of expression, i. e., work of the Agouti gene. While in the norm, this gene is expressed only in skin cells, where it locally influences the fur color, in the mice carrying Ау mutation this gene commences working in all tissues, including the hypothalamus. It appeared that the product of the Agouti gene — the Agouti protein — similarly to the orectic agouti-like protein of the hypothalamus, prevents α-MSH from binding to its receptors. Playing the role of a “voluntary assistant” to ALP, it day by day increases appetite. And chronic overeating anyway leads to inevitable obesity…
Mice of С57Bl/6J strain, which carry Ау mutation, are especially attractive for researchers by that they may be considered as a model of the genetically determined obesity met in humans. Certainly, very few of those people suffering from obesity see a doctor to have their genome studied. However, mutations in various components of the hypothalamic melanocortin system were detected in the majority of those who asked for testing. Thus, the study into the mechanisms of MC obesity and ways of its prevention in mice can have a practical application in the future…
Yellow, fat, and sick… mouse
One should keep in mind that an organism has the peripheral system of body weight regulation along with the central system, localized in the brain. The peripheral system includes various organs, such as liver, muscles, fatty tissue, pancreas, adrenal cortex, stomach, and others. The system responds to the amount and quality of the food consumed and to an increase in the energy consumption connected with physical activity, thermoregulation, and mental activity.
It is known that fatty acids and glucose are the main energy carriers coming with food. A constant level of glucose must always be maintained in the blood (the brain refuses any other energy carriers — glucose only!). The excess energy is stored as fat. The redistribution of energy resources among organs and tissues and their use for the needs of cells are regulated by the hormones of pancreas (insulin and glucagon) and adrenal cortex, the level of free fatty acids in the blood, and many other hormones, fat metabolites, and carbohydrate metabolites.
Obesity disturbs the activity of this system, which regulates the energy homeostasis. In the blood, the levels of leptin, insulin, glucose, and fatty acids increase, while the sensitivity of the target organs to insulin decreases. These impairments called the obesity syndrome result, in turn, in the development of clots, strokes, pathologies of blood circulation, and other diseases. The adult obese yellow mice are no exception — they also develop type 2 diabetes; however, it is not clear what is the cause and what is the consequence. Thus, we decided to study the dynamics of body weight, food consumption, and blood concentrations of hormones and energy substrates in yellow mice with black mice, disinclined to obesity, as control.
So, what has the monitoring of mouse’s life demonstrated? It appeared that already the six-week-old mice are disposed to chronic overeating, which results in a progressive weight gain. With age, the difference between the mice grows, and the 22-week-old yellow females are twice as heavy as the black animals! Such is the result obtained by an insignificant but constant increase in appetite caused by an inappropriate expression of the Agouti protein.
The “symptoms” of obesity in the yellow mice precede the manifestation of the signs of diabetes. During the period of 8 to 11 weeks, females continue to accumulate fat as indicated by an elevated leptin level, but are still similar to the other mice in the rest characteristics. However, already at the age of 13 weeks, their levels of glucose and fatty acids in the blood rise — the first threatening signs indicating to the development of insulin insensitivity, when the tissues lose the ability to capture energy substrates from the blood under the effect of this hormone. Two weeks later, the level of insulin itself increases, as the last attempt to obtain the tissue response, acting not by “skill” but by “number”. Yet all is in vain, after the 15-week age there follows a complete unbalance of the hormonal and metabolic status of the mouse organism. All the characteristics in question reach their maxima: weight, appetite, and blood concentrations of leptin, insulin, glucose, and fatty acids. However, a plenty of glucose in the blood means that it fails to enter the tissues needing it badly, and this is exactly type 2 diabetes.
Any biological experiment gives fewer answers than new questions. It was just our case. Why an “extra” Agouti protein, which is constantly produced in the hypothalamus of yellow mice during the first weeks of their life, has no effect on appetite and body weight? How the fat accumulated in the fatty tissue can prevent the effect of insulin on the cells of other organs? Only further experiments can give the answers.
Pregnant and slim
Another question arises after such experiments: Is it possible to prevent obesity development? Unfortunately, despite a notable breakthrough in our understanding of the mechanisms underlying obesity development, almost nothing is known about possible ways of its reduction.
While breeding yellow and black mice at the vivarium with the Institute of Cytology and Genetics SB RAS, Dr. E. N. Makarova noticed that yellow females did not gain excess weight when during pregnancy and nursing of their offspring. This observation drove us to perform a special experiment. It appeared that if a yellow female conceived soon after reaching puberty (at the age of 8 weeks), it lost its excess grams by the end of the pregnancy and virtually did not differ in weight from the always slim black individuals by the end of lactation.
What is the reason of this amazing phenomenon? First, we assumed that the fertility capacity of yellow females was possibly higher, and they spent more energy for nursing their litter; that is why they did not gain excess weight. However, tests demonstrated that this was not the case.
Birth and nursing of the offspring relieved the females with genetically determined obesity, at least, temporarily, from obesity and the related diabetesThen we studied the effect of pregnancy and lactation of yellow females on their appetite and characteristics of carbohydrate–fat metabolism. Usually, appetite increases during pregnancy, especially its second half, when the fetus grows intensively. That is when something breaks in the mechanism of action of the Ау mutation: the yellow females commence undereating black mice! As a result, the yellow and black mice reach the time of delivery with equal body weights. It is also a surprise that later, during nursing, the yellow females were virtually similar to the black females with normal metabolism in food consumption and metabolic characteristics.
So, what happens with Ау mutation during pregnancy and lactation — specific physiological states, which only the “fairer” half of the species can experience? The females lack any physiological system whose function would not change during reproduction. A considerable exertion in this process falls also on the system of energy balance regulation. While for the males the energy expenditures for reproduction in the majority of species cease with fertilization of the egg cell, they only start for the females. And these expenditures are huge! In small mammals, the appetite of females, especially during lactation, increases three–fourfold! A nursing mouse with a body weight of 26—28 g eats daily 12—14 g of food, that is, half its own weight. Such food consumption is a hard labor. A strongest nutrition motivation must exist, aimed at an increase in appetite to degree that would compensate for enormous energy expenditures resulting from milk production.
Indeed, it has been demonstrated that the production of appetite-stimulating peptides, including ALP, similar in its structure and properties to the Agouti protein, considerably increases (Chen et al., 1999). We assume that the production of this appetite-stimulating protein during lactation is so high that it completely blocks the binding of the anorexigenic melanocyte-stimulating hormone to hypothalamic receptors, thereby multifold increasing the consumption of food by all mice without exception. On the background of such a powerful physiological stimulation of appetite, an increase in the food eaten due to the Ау mutation and its effect on the body weight is just “lost”. We are planning to test this hypothesis experimentally in the near future.
Wanna be healthy? Reproduce!
The last but not idle question is left to be answered: For how long does the “health-improving” effect of the reproductive function on metabolism continue? We measured the hormonal metabolic characteristics of the parous yellow females almost two months after the completion of lactation and found that all characteristics are virtually normal at the age of 22 weeks. Thus, we may state that the birth of offspring relieved yellow mice, at least temporarily, from obesity and, as consequence, type 2 diabetes. However, still many experiments will be necessary to explain this phenomenon.
To conclude, let us return to humans and their problems associated with obesity. Our results allow if not solving but at least having a new look at them. For example, it is a widespread opinion that pregnancy and lactation ruin the woman’s figure. However, we came to know that the situation is opposite, at least for mice.
Similar to mice, the woman after delivery has a multitude of stimuli for milk production, from hormonal regulation to the very look of her baby, his/her cry, and smell. The appetite of a nursing woman drastically increases to compensate for the energy spent on milk production. And if a woman succeeded in breastfeeding for a long period, nothing threatens her figure. However, if the appetite increased after delivery is combined with reluctance or impossibility to breastfeed, excess kilos are guaranteed. However, it is not lactation that should be blamed, but its absence.
Presumably, the time will come sooner or later when all people suffering with obesity are mandatory tested for the presence of mutations affecting the melanocortin system of the brain. It cannot be excluded that young women from the families predisposed to development of this type of genetic obesity will make use of the information obtained in yellow mutant mice: to avoid obesity, they will bear and breastfeed children. Would not you agree: it is much better to spend your energy for raising your children than to plough the sand combating the overweight?
* There is a widely known Russian saying: eat your breakfast yourself, share your dinner with a friend, and give your supper to an enemy
References
Bazhan N. M et al. Changes in the carbohydrate – fat metabolism during development of melanocortin obesity in mice with Agouti yellow mutation, Ross. Fiziol. Zh. Im. IM Sechenova, 2005, in press.
Cone RD et al. The arcuate nucleus as a conduit for diverse signals relevant to energy homeostasis, Int. J. Obes. Relat. Metab. Disord., 2001, v. 25, Suppl 5, p. S63—S67.
Bultmann et al. Molecular characterization of the mouse agouti locus, 1992, Сell, v. 71, p. 1195—1204.
Chen P et al. Altered expression of agouti-related protein and its colocalization with neuropeptide Y in the arcuate nucleus of the hypothalamus during lactation. Endocrinology, 1999, v. 6,
p. 2645—2650.
The research was supported by the Russian Foundation for Basic Research (grant no. 04-04-48760).
Dr. Sci. M. P. MOSHKIN, Institute of Animal Systematics and Ecology SB RAS (Novosibirsk) comment
The size is important
The slogan “Wanna be slim? Reproduce!” will hardly become popular in the densely populated countries of Southeast Asia. However, in Russia, where the population is steadily declining, while the percent of women with overweight is increasing, this conclusion of scientists meets the most cherished beliefs of both common people and statesmen. And this is not a frequent case.
A relative decrease in the body weight observed in reproducing mouse females with genetically determined obesity additionally combined with a suppressed appetite is indeed an intriguing fact, which generates a number of questions. First and foremost, the weight loss after delivery and breastfeeding contradicts our everyday experience, enriched with directly opposite examples. What is the reason of such striking distinctions between species?
An important circumstance that determines the specific features of bioenergetics of different species is the body size. As for small mammals (for example, 6-gram fingerling ,—lesser white-toothed shrew Crocidura suaveolens), the weight of newborns may reach 50 % and more of the weight of their mothers. With an increase in the size of adult individuals to 10 kg and more, the relative weight of their newborns usually does not exceed one tenth of the mother’s weight. Humans as a biological species fit in this rule: the relative size of the newborn children falls into the range corresponding to the human size class.
The larger is the relative body size of the offspring, the higher, respectively, are the energy expenditures of the mothers. Here, it is necessary to take into account the fact that since small animals have a disadvantageous ratio of the body surface to the volume from the standpoint of heat loss, the intensity of the energy metabolism per unit body weight also increases with a decrease in the animal size. Therefore, the energy expenditures of small animals are high everywhere. Although the change in their ability to assimilate essentially the food energy has the same trend, nonetheless they cannot keep up with the growth in a relative size of their kids.
The effect of all these factors in the species whose body weight is below 1 kg results in that pregnancy and nursing proceeds under a negative energy balance of the maternal organism. The bottleneck limiting the energy supply of pregnant females is the gastrointestinal tract (Wainer, 1987, 1992). They “haven’t got the guts for it”. Humans, as well as other mammals with a body weight exceeding 10 kg, have no such problems; hence, pregnancy may be accompanied with fat accumulation in the mother’s body.
Thus, if a decrease in the body weight of pregnant mice results from the energy patterns, then what “forces” females with genetically determined obesity to reduce feed consumption? The paper by N. M. Bazhan gives the answer in part; however, it provides an explanation from the physiological standpoint only. Is it possible to find any adaptive sense in such an appetite reduction?
A logical analysis of the significance of a biological phenomenon (in other words, substitution of natural selection with one’s own estimations) is a speculative matter yet of some use. As in all philosophical issues, here it is better to rely on authorities, for example, Richard Dawkins. Once acquainted with his book “The Egoistic Gene”, it is easy to agree that a pregnant and nursing female as a “machine for gene survival” is of a higher value than a nonpregnant one. From this standpoint, a female bearing 10 descendants becomes sixfold more valuable, as each kid carries half the maternal genome. Therefore, if the fat reserves accumulated before pregnancy are sufficient for the bearing and nursing of the offspring, is it of any use to risk to go and seek for feed? This is a rather dangerous affair in the real life of mice (and not only mice!), as they can encounter with a predator, poisoning, food infection, and so on. In this sense, even pathological obesity of the mother can be regarded as an extreme manifestation of adaptation directed to the safe provision of the future progeny.
Note that many non-communicable diseases have similar adaptive roots. Moreover, the particular pathogenic mechanisms of “diseases of adaptation” are extremely diverse. Thereupon, we may congratulate the author and her colleagues that they succeeded to enter the promising way for studying the mechanisms of melanocortin obesity, affecting many people, and developing approaches for its correction.