Smallpox: Damocles’ Sword of Civilizations
Smallpox, frequently referred to as the curse of mankind, was successfully eradicated 35 years ago owing to mass vaccination and strict antiepidemic surveillance. This is the first and so far unique case of a global liquidation of a most dangerous infectious disease by the joint efforts of the world community. However, the questions remain whether smallpox disappeared for good and another smallpox-like infection can emerge again. The answers to these questions require the knowledge of when this pathogen emerged and how it had adapted to the human body as well as the insight into the mechanisms underlying coevolution of pathogens and their hosts
Smallpox or variola (not to be confused with chickenpox) is a special infectious disease, which has taken heavier toll of human lives than any other infection and even wars.
The pathogen causing smallpox induced most pronounced clinical manifestations and caused so large-scale epidemics with a high mortality rate that many historians and physicians left documentary evidences about this disease. Although the extant records are fragmentary and scattered as well as not always allow for a reliable cause of particular epidemic outbreak, it is safe to state that this disease has spanned a vast territory from Egypt in the west to China in the east.
Since the days of crusades, epidemics of this devastating disease broke out over the European continent on a regular basis being imported from the Near East: in the 6th–7th centuries, smallpox outbreaks were recorded in France, Italy, Spain, and other European countries. The first heard of severe smallpox epidemics in Russia date back to the 15th century, becoming so common in Europe starting from the next century that only the cases of extraordinary large epidemics deserved the attention of annalists.
The incubation period from the moment of infection to the onset of fever is usually 10 to 14 days. The disease has two main stages, namely, prodromal (before development of rash) and eruptive stages.
The first stage continues for 2–4 days with high body temperature (up to 40.5°C), severe headache, characteristic low back pain, tachycardia, breath acceleration, nausea, sometimes vomiting, and raving.
Then body temperature decreases, and skin eruptions as small reddish knots (papules) develop first on the face and arms and then on the other parts of the body. Increasing in number and size, papules develop into vesicles with transparent contents and a characteristic depression in their center. By days 6–7, vesicles become purulent (stage of pustules), which is accompanied by the new increase in body temperature. On day 10–13 of the disease, pustules reach their maximum size and start to gradually flatten, dry, and form scabs, which drop off by days 30–40 of disease, leaving reddish spots.
Later, characteristic skin depressions, pockmarks, are developed instead of spots on some parts of the body (mainly on the face, resulting in the so-called pitted face).
Those who recovered from smallpox acquire a life-long immunity to this disease and are not chronic variola virus carriers.
Even in the 20th century, that is, over incomplete 80 years of mass antismallpox vaccination and intensive control of this disease involving strict quarantine measures, smallpox killed at least 300 million people.
Coevolving
Similar to the other viruses, variola virus is unable to exist independently, requiring higher host organisms sensitive to them for their reproduction. Note that the genetic programs of both the viruses themselves and of their hosts are constantly changing and their optimal variants are selected. The only difference there is in that the viruses reproduce in an infected cell of the host body over a short time span (several hours) and generate most numerous progeny (hundreds and thousands of daughter virus particles).
 Multicellular organisms, such as humans, cannot be compared with viruses in the reproduction rate and efficiency. When an epidemic develops in a real human population, which remains genetically unchanged over this short period, the virus spreads from individual to individual following a chain reaction principle. Such a process may lead to emergence of numerous mutant (altered) variants of the initial virus and selection of a variant that under the particular conditions displays advantages in spreading and reproduction. If the infection ends in a lethal outcome, the most sensitive individuals die. In this process, there are always individuals rather insensitive or even resistant to the corresponding infectious agent.
Multicellular organisms, such as humans, cannot be compared with viruses in the reproduction rate and efficiency. When an epidemic develops in a real human population, which remains genetically unchanged over this short period, the virus spreads from individual to individual following a chain reaction principle. Such a process may lead to emergence of numerous mutant (altered) variants of the initial virus and selection of a variant that under the particular conditions displays advantages in spreading and reproduction. If the infection ends in a lethal outcome, the most sensitive individuals die. In this process, there are always individuals rather insensitive or even resistant to the corresponding infectious agent.
Susceptibility to infection is determined by specific genetic features of individuals; therefore, not only new virus variants emerge during mass epidemics, but also the host population becomes enriched for the individuals with genetically specified resistance to the corresponding virus. This is how a virus and its host coevolve in an interdependent manner, taking into account that the evolutionary rate of the viruses is considerably higher as compared to the analogous process of animals and humans.
An important specific feature of smallpox is in that it is a strictly anthroponotic infection, i.e., the infection with a human-to-human transmission; currently, there are no other mammalian species sensitive to this pathogen. In addition, this infection is highly contagious, i.e., it is readily and efficiently transmitted from infected to healthy persons. Presumably, variola virus originated from a virus able to infect a wider range of sensitive animal hosts but lost this ability during its evolution and maximally adapted to the human body (Shchelkunov et al., 2005).
A never-ending circle
Once an acute infectious disease is able to rapidly spread in a host population soon leading to death or recovery with acquisition of immunity, the outbreak should rather quickly deplete the “reserve” of sensitive individuals. If in such a case the corresponding pathogen loses the ability to reproduce in its earlier existing natural reservoir, that is, in feral animals, than the epidemic will soon fade in a relatively small and sparse population.
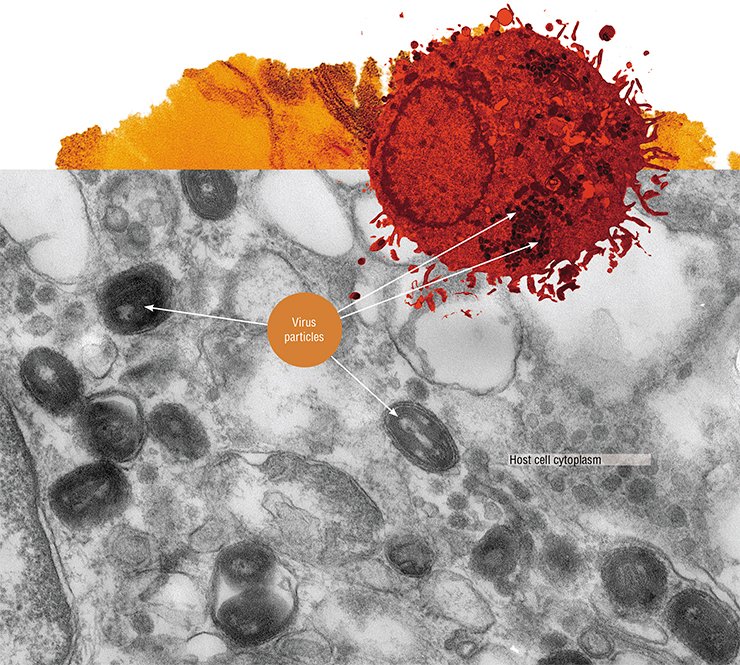
The genome of variola virus is a linear double-stranded DNA molecule comprising 187 kilobase pairs (kbp) with covalently closed hairpin structures at both ends. The genome contains about 200 genes; this is a tremendous number as compared with the majority of viruses belonging to the other families. The virus particles have several lipoprotein envelopes and numerous structural proteins as well as the enzymes necessary for virus reproduction in the host cell.
The overall cycle of variola virus development takes place in the host cell cytoplasm within specialized structures, referred to as virosomes or virus factories
As for a large human population with its high density, infection can travel from one area to another, coming back to its initial focus many years after, when the new generation sensitive to the corresponding pathogen was born and grew up. In this case, an anthroponotic infection will be maintained in a certain territory for many years, attaining the so-called endemic state.
The most ancient extant smallpox descriptions, dated back to the 4th (China) and 7th (India and Mediterranean) centuries, define this disease first and foremost as a childhood infection with a low mortality rate among children. This suggests that smallpox as early as that time was stably endemic in these densely populated geographic regions.
In India, despite a centuries-long endemicity of this disease and a long-term coevolution of variola virus and population of this region, the children’s mortality rate among unvaccinated individuals before 5 years old during periodic epidemics could reach 50% even in the 20th century (Fenner et al., 1988). This stems from the fact that variola virus has a multifactorial system providing for overcoming of numerous defense responses of the human body directed against infectious agents (Shchelkunov, 2011, 2012). Thus, the probability that the human population could genetically adapt to this virus thereby considerably decreasing its pathogenicity is extremely low.
Over the passed centuries, the evolution has to the greater degree altered the virus itself. Note that the smallpox epidemics that broke in the most densely populated and vast areas (the Indian subcontinent) displayed the highest mortality rate versus lower mortality in the areas with sparser population.
From animals to humans
 It is known that the majority of human pathogens originate from zoonotic (that is, characteristic of feral animals) infectious agents. Moreover, many viruses do not cause any pronounced disease in their natural hosts but may be highly pathogenic when infecting another species, human included. Marburg and Ebola viruses, whose natural host is African bats, are among the most illustrative example. These viruses do not cause any disease in bats even after a laboratory infection at a high dose but lead to most severe hemorrhagic fevers with a mortality rate up to 80% in humans.
It is known that the majority of human pathogens originate from zoonotic (that is, characteristic of feral animals) infectious agents. Moreover, many viruses do not cause any pronounced disease in their natural hosts but may be highly pathogenic when infecting another species, human included. Marburg and Ebola viruses, whose natural host is African bats, are among the most illustrative example. These viruses do not cause any disease in bats even after a laboratory infection at a high dose but lead to most severe hemorrhagic fevers with a mortality rate up to 80% in humans.
Establishment of large populations of domestic animals had most important role for the infectious “history” of the mankind. The animals involved in close and frequent contacts with humans are typically the effective intermediate reservoir for transmission of a pathogen from wild animals to humans.
In this process, most of zoonotic pathogens at the initial stages are unable to be transmitted from an infected person to a healthy one. However, with an increase in the rate of new host infection such a virus via a natural evolution may acquire the ability to be efficiently transmitted between human individuals and thus become the cause of epidemics. The period for complete adaptation of a virus to its new host and transformation into an epidemically dangerous pathogen may sometimes take many years (Shchelkunov, 2011).
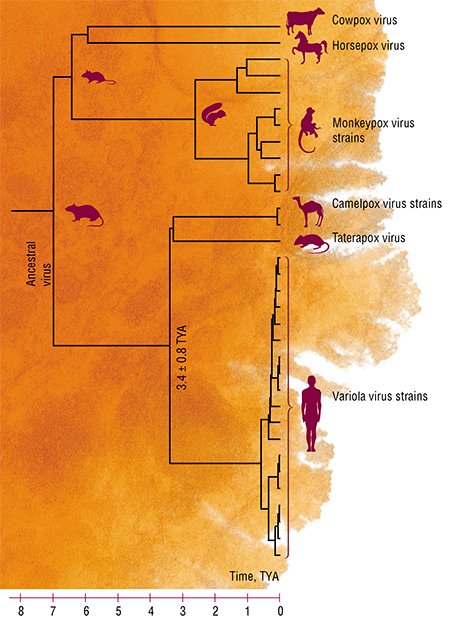
The genome-wide sequencing of viruses have allowed the speciation and independent evolution time spans to be estimated for various orthopoxviruses, including variola virus (Babkin and Shchelkunov, 2008). It has emerged that the “related” variola and camelpox viruses originated from a common ancestral orthopoxvirus (presumably, a rodent virus) approximately 3.4 ± 0.8 thousand years ago (TYA) and then independently continued their evolution.
Conceivably, this ancestral orthopoxvirus, which had a wide host range, acquired the ability to infect humans about 4 TYA. Moreover, it caused only skin lesions without any severe consequences in both humans and their domestic animals. Along the trade routes of ancient civilizations, the virus could spread over a tremendous area spanning from the Indian subcontinent to the Nile River valley causing there sporadic outbreaks of a relatively mild infection. However, with its adaptation to the human body, the outbreaks could become more massive, in turn, leading to emergence of new virus variants (Shchelkunov, 2009).
The first advents
СIt is believed that smallpox appeared somewhere in Egypt (Near East); however, numerous extant written sources of that time do not mention any epidemics of this disease. Thus, it is reasonable to consider an alternative variant associated with the history of highly developed ancient Indus Valley (Harappan) Civilization, discovered by archaeologists only in the 1920s (Al’bedil’, 1991).
About 2500 B.C., the cities very large for that time appeared in the long valley of the Indus River; their population by the end of the 2nd millennium B.C. amounted to approximately 5 million people. However, these cities became deserted by 1.8–1.6 B.C. due to unknown reason. There are no evidences of any relevant wars or natural cataclysms; moreover, numerous remains of human corpses carrying no evident signs of wounds or injuries were found when excavating the largest city of Mohenjo-Daro; this is even more surprising, since according to archaeological data, cremation of dead was characteristic of this culture.
The most apparent explanation for the collapse of the Indus Valley Civilization, one of the three most ancient civilizations of mankind along with the Ancient Egypt and Sumerian ones, is an epidemic of a fatal disease. The origin of variola virus (3.4 ± 0.8 TYA) matches well the period when the ancient Indus Valley population dramatically decreased (3.8–3.6 TYA); this suggests that smallpox might be the particular mortal infection causing mass epidemics among this population, lacking immunity to the disease, and eventually led to this devastation (Shchelkunov, 2009). Most likely, the size of this human population prevented smallpox to become an endemic disease, and this infectious agent, highly pathogenic for humans, disappeared.

However, its zoonotic ancestor (or a low virulent variola virus variant with a wide host range) most likely continued to circulate in the natural reservoir (rodents) over a large area. Such a situation is characteristic of any new highly lethal human infection: the best known example is the Spanish flu epidemic of 1918–1919.
THE GODDESS WHO COOLSDespite some variation in the iconography, Shitala is easily recognizable: she is represented riding an ass either nude or dressed as a married woman, frequently as an old Brahmin woman, crowned with a winnowing-fan and carrying a broom and a pot with water in her hands.
It is likely that the worship of this goddess was established rather late: the first mentions of her appeared in medical treatises of the 16th century, although the description of the disease is found in the manuscripts dated back to long before Christ.
Many signs suggest that the worship of Shitala is folkish in its origin not immediately adopted by the Hindu religious concepts. In particular, Shitala is not mentioned in early Brahmanas and the worship of Shitala is mainly conducted not by Brahmins, but rather by low caste pujaris, Malakars.
In some places, bloody sacrifices are still offered to this goddess, although in general Shitala prefers bloodless gifts, such as coconuts, cold rice, sweets, and other “cooling” foodstuff.
The goddess, who was born from the cooled ashes of the fire of sacrifice, hates heat and always searches for freshness, awarding those who will succeed in conciliating her and punishing the lazy adherers with the heat of smallpox. It is not surprising that smallpox in this concept was not regarded as a dangerous disease but rather as a manifestation of the presence of the angry goddess. That is why a smallpox patient—a poor victim of the goddess indignation—was first and foremost healed by cooling his/her body with cold drinks, fanning with punkahs, and sponging body with ice-cold water or moistened leaves of the neem tree, the favorite tree of the goddess, actually known to be efficient against many skin maladies. All these actions were accompanied by songs addressed to Shitala.
The highest mortality rate of smallpox was recorded in India during dry months of the year, from February to April, and drastically decreased by the beginning of rainy season. That is why smallpox in India was frequently called a spring disease and Shitala, correspondingly, spring goddess (the major festival worshiping her is in mid-March).
Even now, any “heating” actions are prohibited during her festival to avoid the anger of “cooling” goddess, namely, cooking hot meals, using spices, and setting up sacrificial fire in houses, as well as any martial relations.
Although the name of this goddess is first associated with smallpox, her person is rather intricate. For example, Shitala also protects children and grants luck. Despite specific details in the worship of Shitala in different localities, her main feature is unchanged—she cools (Shitala literally means in Sanskrit “the one who cools”).
Now the “cool” goddess is much more than a mere local goddess protecting from smallpox: she is a symbol and a constant reminder of the need to observe a correct balance between heat and cold in the human body. A disturbance of such balance, drawing the ire of goddess, may lead to onset of a dangerous disease.
of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences, St. Petersburg, Russia
The researchers of ancient manuscripts, including the Talmud and Bible scholars, have not found there any described epidemics of a strictly anthroponotic infection with skin eruptions resembling smallpox. However, relying on our above assumption that the smallpox agent originated from an orthopoxvirus with a wide host range, which at the initial stages of its adaptation to human host retained its properties of a zoonotic infection with a low pathogenicity for humans, the description searched for is found in the Bible being related to the exodus of Israelites from Egypt (14th century B.C.): “...there shall be boils and swelling blains both in men and beasts, in the whole land of Egypt” (The Exodus, Chapter 9).
The indigenous population of America had never encountered this infection, and smallpox became a catastrophe for them: some tribes were almost completely wiped off. It is known that only the smallpox epidemic of 1520 in Mexico swept off about 3.5 million lives! It was not until several large smallpox epidemics had come over both American continents that the disease became endemic with a low (less than 1%) mortality rate.
By the time of Columbus landing, the population of South and North Americas was approximately 70 million people; however, the subsequent epidemics and, to a considerably lesser degree, wars reduced this population to 600,000 people by the year of 1800.
 This demonstrates that epidemics of a zoonotic infection affecting both humans and their domestic animals with characteristic skin eruptions on their bodies but not accompanied by a lethal outcome took place in ancient times in Egypt and the Near East (Shchelkunov, 2011).
This demonstrates that epidemics of a zoonotic infection affecting both humans and their domestic animals with characteristic skin eruptions on their bodies but not accompanied by a lethal outcome took place in ancient times in Egypt and the Near East (Shchelkunov, 2011).
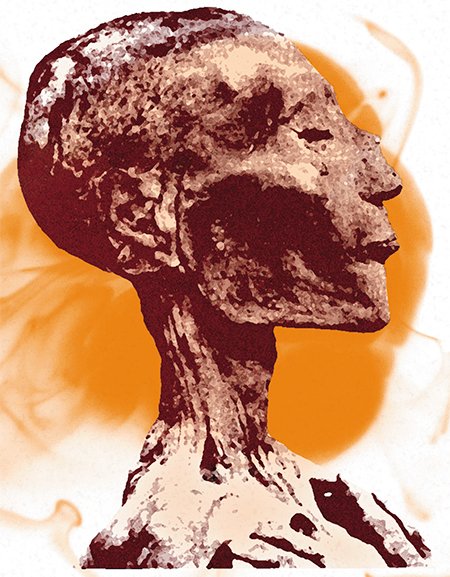
It cannot be excluded that a mysterious catastrophe of the Bronze Age in the Near East and Eastern Mediterranean dated back to 1200–1100 B.C. was also associated with an epidemic of smallpox but at that time with a high mortality rate. Characteristic of this period was a drastic decrease in the size of human population living there, destruction of cities, and catastrophic changes in social pattern (Robbins and Manuel, 2001). Two of the three discovered Egyptian mummies with the skin lesions typical of smallpox belong to this particular period (Fenner et al., 1988).
Presumably, the virus dangerous for humans re-emerged at that time in the Near East and Eastern Mediterranean region, housing several million people; however, an insufficient size of the human population again interfered with endemization and preservation of this new anthroponotic infection.
The next advent of smallpox took place in the middle of the 1st millennium B.C. in the Indian subcontinent. There, in the Ganges Valley, the largest and densest human population (about 25 million people) had established by that time. It is likely that such a population density was sufficient for the newly emerged highly pathogenic virus to become endemic.
At that time, Greece was the most densely populated among the European countries, with the total population of approximately 3 million people by 400 B.C. Most likely, smallpox was unobservable in both Greece and the Near East; at least no smallpox epidemic took place in the army of Alexander the Great on its way from the Mediterranean Sea to India. However, a disease with the skin lesions characteristic of smallpox broke out when this army stayed in the Indian subcontinent in 327 B.C.
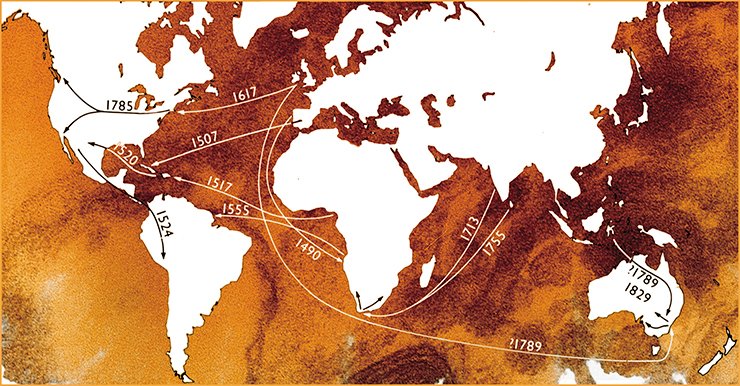
Smallpox endemization in the Indian subcontinent provided for preservation of this agent, highly pathogenic for humans, over many centuries until the 20th century. From this area, the disease gradually spread over the whole world, being successfully eradicated only in the second half of the last century with the help of prophylactic vaccinations.
Fighting fire with fire
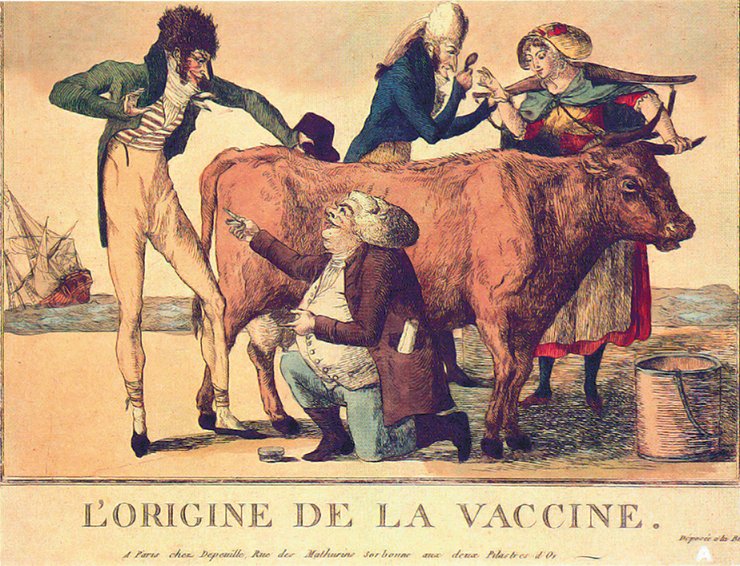
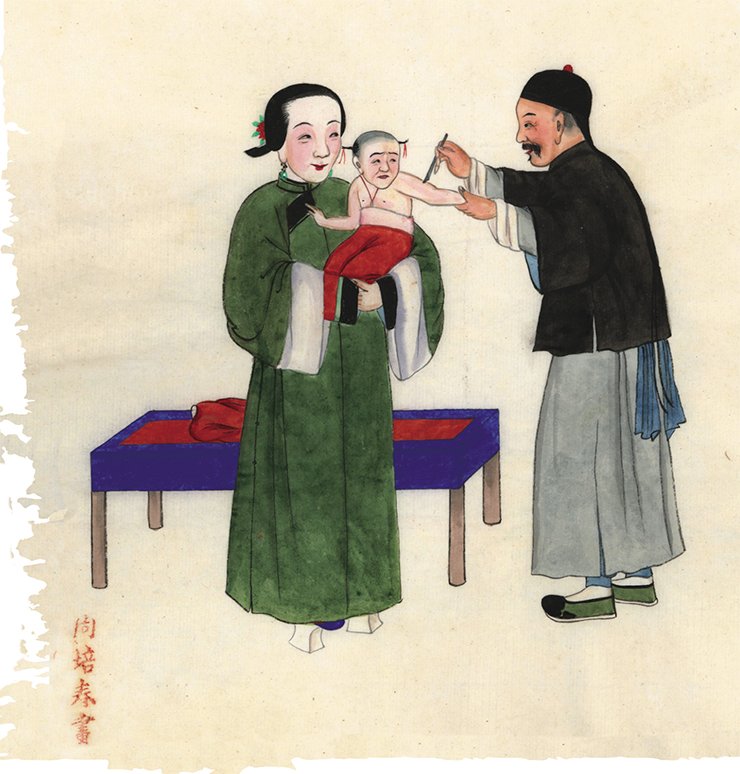
Note that smallpox-like diseases have been known in livestock (cows, horses, and buffaloes) since ancient times. It was observed that the people contacting sick animals had the same disease in a milder form, only with skin lesions. But on the plus side, such people became unsusceptible to the lethal infection during smallpox epidemics.
Based on such observations, Edward Jenner, an English physician, was the first to propose in 1996 to inoculate the infective element from sick cow or horse pustules as the protection from smallpox. This method for protection against smallpox was referred to as vaccination (from vache, the French word for cow); later, this term was applied to immunization against any infections.

Note that the kingdom of viruses was discovered a century after the vaccination against smallpox was adopted. Although the nature of the protective agent was unknown at that time, the antismallpox vaccination was actively used first in Europe and then around the world.
Initially, people were inoculated with infectious material taken directly from sick cows or horses by introducing it into the body through scratches on the forearm skin. Later, the material for vaccination was taken from the skin lesions on the forearms of vaccinees, referred to as an “arm-to-arm” method.
In the second half of the 20th century, it became possible to produce the vaccination material in quantity from the calves infected by mass skin scarification. This allowed the vaccine preparations to be standardized and mass vaccinations against smallpox to be implemented (Fenner et al., 1988).
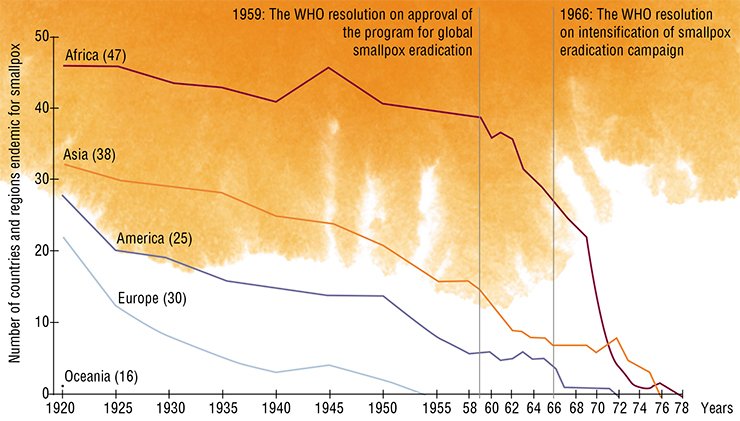
In Russia (USSR), smallpox vaccination was mandatory since 1919. This allowed the dangerous disease to be eradicated over a stunningly short time span (by the year of 1936!) in the country with tremendous territory and most diverse geographic zones, from deserts to northern tundra, housing dozens of ethnic groups with different traditions and convictions.

Many developed countries acted in the same manner in the first half of the 20th century. Nonetheless, smallpox outbreaks were annually recorded in the 1950s in 50 to 80 countries of the world, while the endemic smallpox foci in Asia, Africa, and South America could pose a menace to the countries already free of this infection. That is why even these countries were involved into antismallpox vaccination.
The turning point took place in 1958, when V.M. Zhdanov, a deputy minister of public health, proposed on behalf of the Soviet Union delegation at the 9th Session of the World Health Assembly to initiate the global smallpox eradication program. The corresponding resolution was approved on June 12, 1958, launching the unprecedented international global smallpox eradication campaign.
SMALLPOX “BEHIND BOLT AND BAR”The laboratories of these centers are equipped to guarantee complete safety both for the manipulations with these viruses during research and for environment. International WHO commissions visit these laboratories on a regular basis to control the organization of experimental works with viruses and state of the engineering systems providing this safety.
The currently conducted experiments with variola virus are first and foremost aimed at the search for efficient antivirals and design of state-of-the-art safe antismallpox vaccines
All the applications for the studies of this type obligatory undergo expert reviews in the WHO research subcommittee for smallpox, and only the projects important for public health are approved. The experimental results obtained at the Russian and American Collaborating Centers are annually reported to the WHO Consultative Committee on Smallpox Research at the WHO headquarters in Geneva (Switzerland)
The Soviet Union not only was the initiator of this program, but also rendered manifold assistance at all stages of its implementation during the subsequent years. As early as in 1958, the Soviet Government supplied 25 million doses of dry antismallpox vaccine to the WHO to be dispensed in different countries. Two years later, a specialized laboratory was organized with the Moscow Institute for Viral Preparations aimed at large-scale production of the antismallpox vaccine meeting the WHO requirements. This laboratory also became the center for training foreign specialists. During the two decades of this international campaign, this country supplied more than 1.5 billion antismallpox vaccine doses, used for mass vaccinations in 45 countries.
The last case of smallpox was recorded in 1978, and two years later, the 33rd WHO session triumphantly declared that the world and all its nations had gained the victory over smallpox. Concurrently, all the countries were recommended to cease vaccinating the population against smallpox.
However, the question on whether this dangerous infectious disease is liquidated for good still remains after this victory.
The answer is not so simple. Potential menace of smallpox “rebirth” still remains, since close relatives of variola virus, the zoonotic orthopoxviruses pathogenic for humans, are abundant over vast areas in Eurasia, Central Africa, and South America. These virus species include monkeypox, cowpox, buffalopox, and vaccinia viruses, the natural reservoirs of which are various rodent species (Shchelkunov et al., 2005).
In particular, outbreaks of the disease caused by buffalopox virus involving thousands of animals and hundreds of people have been recently recorded in India. If this situation is left to take its course, ever more people will be infected by the virus with an increase in outbreaks, allowing the virus to completely adapt to the human body and turn into an epidemically dangerous infectious agent.

However, there is yet no basis for panic: the current situation is fundamentally different from those in the far past. All outbreaks of human and animals orthopoxvirus infections are now recorded and investigated by medical and veterinary experts as well as the strategies of vaccination and antiepidemic activities for such infections were worked out during the global antismallpox campaign.
All the local outbreaks of human orthopoxvirus infections should be controlled with the help of state-of-the-art rapid species-specific diagnostics as well as quarantine and vaccination should be used to prevent their growth into epidemics. Smallpox will not return provided sufficient wisdom and the proper efforts of the WHO and the medical services of the countries involved in the control of livestock and human orthopoxvirus infections.
References
Babkin I. V., Shhelkunov S. N. Molekuljarnaja jevoljucija poksvirusov // Genetika. 2008. T. 44, № 8. S. 1029—1044.
Shhelkunov S. N. Protivovirusnye vakciny – ot Dzhennera do nashih dnej // Sorosovskij obrazovatel’nyj zhurnal. 1998. № 7. S. 43—50.
Shhelkunov S. N. Preodolenie ortopoksvirusami zashhitnyh sistem organizma mlekopitajushhih // Molekuljar. biologija. 2011. T. 45, № 1. S. 30—43.
The Editorial Board is grateful to Ya.M. Vasil’kov and K.M. Vozdigan, Museum of Anthropology and Ethnography (Kunstkamera), Russian Academy of Sciences, St. Petersburg, for their assistance in preparing the manuscript for publication