Antibodies against Carcinogens
In fact, it is fundamentally impossible to create a universal vaccine against cancer, a wily and multifaceted disease. A healthy lifestyle and good ecology are the only factors at our disposal. However, impressive successes in the vaccine prevention of infectious diseases have given rise to a hope of creating vaccines against chemical carcinogens, i.e. substances that induce development of malignant neoplasms. First and foremost, such carcinogens are the combustion products of organic fuel in industrial discharge
In the majority of developed countries of the world, including Russia, cancer diseases are second in the list of mortality causes after cardiovascular diseases. However, atherosclerosis and hypertension can be treated for years and decades, whereas cancer is dreaded disease because of its fulminant character: every third patient dies within a year since cancer has been diagnosed.
The main efforts of researchers to control malignant tumors are focused on improving the old healing methods and developing the new tools; however, the fundamental postulate of medicine that it is easier to prevent a disease that to treat it still remains no more than a postulate. There are currently no pharmacological tools for cancer prevention that can be comparable in their efficiency to those for prophylaxis of infectious diseases. First and foremost, the reason is the multifactorial nature of malignant neoplasms, which implies a multitude of possible causes and a diversity of mechanisms underlying tumor development. This specifies almost insurmountable difficulties in solving the problem of cancer prevention in each particular case.
However, although there are no universal tools for cancer prevention, the designing of drugs that can affect individual factors and components in the pathogenesis of cancer diseases looks quite feasible.
Industrial Kuzbass
According to the experts from the International Agency for Research on Cancer (IARC), the main cause of this disease is the environmental factors of chemical nature. These are carcinogens, that is substances whose impact elevates the rate of malignant tumor onset and/or accelerates their growth in human or animal population in a statistically significant manner. The most widespread carcinogens in the industrially developed countries are the combustion products of organic fuel.
According to the IARC lists and the Sanitary and Epidemiological Guidelines and Standards of the Russian Federation, coal contains and/or generates during combustion several carcinogenic substances, including benzopyrene; benzanthracene; coal tar resins; beryllium, cadmium, arsenic, nickel, and their compounds; dioxin; and radon. Correspondingly, a carcinogenic hazard of various industrial processes such as coke production, processing of coal tar resins, coal gasification, and manufacture of cast iron, steel, and aluminum has been doubtlessly proved.
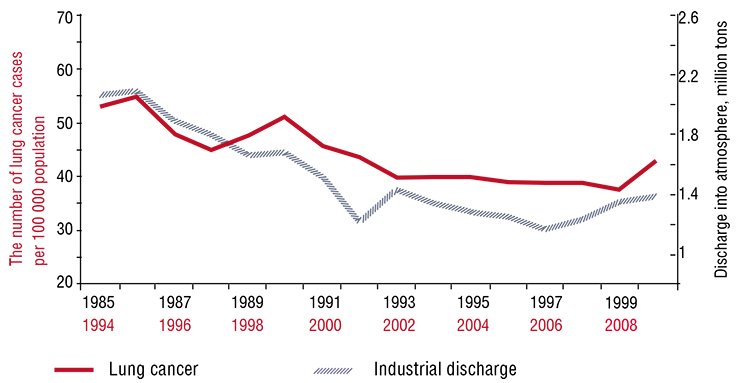
 Kuzbass, which is the main coal mining region of Russia, providing 56 % of mining, 19 % of rolled stock, and 15 % of steel in this country, occupies only 2 % of its area. The ecological consequences of such a high concentration of heavy industry are notorious: the annual industrial discharge into the atmosphere over the last 25 years has been about two million tons and the wastewater discharge into aquatic bodies, 1.3 million tons.Thus, each inhabitant of the Kemerovo oblast “receives” from 0.5 to 1.2 tons of pollutants to say nothing about the amount of industrial waste accumulated in numerous waste dumps.
Kuzbass, which is the main coal mining region of Russia, providing 56 % of mining, 19 % of rolled stock, and 15 % of steel in this country, occupies only 2 % of its area. The ecological consequences of such a high concentration of heavy industry are notorious: the annual industrial discharge into the atmosphere over the last 25 years has been about two million tons and the wastewater discharge into aquatic bodies, 1.3 million tons.Thus, each inhabitant of the Kemerovo oblast “receives” from 0.5 to 1.2 tons of pollutants to say nothing about the amount of industrial waste accumulated in numerous waste dumps.
Studies of the researchers from the Institute of Human Ecology, Siberian Branch, Russian Academy of Sciences (Kemerovo, Russia), have demonstrated that morbidity rates for lung and gastric cancers in the Kemerovo oblast directly correlate with the volume of annual pollutant discharge into the atmosphere and aquatic bodies (an analogous pattern is characteristic of the Donetsk Oblast, Ukraine). According to statistical data, for the lung cancer morbidity rate to be under 40 cases per 100 000 population and for gastric cancer, no more than 26 cases, the volume of industrial pollution of the atmosphere and aquatic bodies should not exceed 1.2 and 0.5 million tons, respectively.
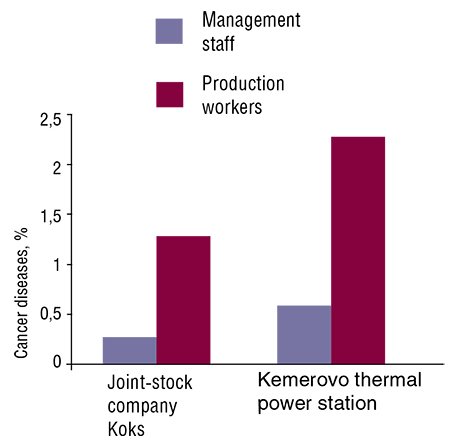
It has also been found that the rate of malignant tumors developing in the workers directly involved in the production processes at the coal processing plants Koks joint-stock company and at the Kemerovo thermal power station is considerably higher as compared with that typical of the auxiliary staff. In addition, these workers also display a statistically significant increase in the rate of chromosome aberrations (rearrangements) as compared with the staff not directly involved in the production process (Estimation and Prediction of Carcinogenic Hazard, 2010).
Protective biotransformation
Polycyclic aromatic hydrocarbons are the most widespread and best studied chemical carcinogens, which are frequently referred to as procarcinogens since, being chemically inert, they are unable to interact with DNA and to directly cause cell malignization. However, owing to their hydrophobicity they are able to impair the structure and functions of the lipid membranes surrounding the most important intracellular organelles.
Therefore, these hydrocarbons are subject to biotransformation in the cells of many body tissues. Initially, they are transformed into water-soluble compounds, which, due to chemically active groups appearing in their structure, acquire the ability to covalently bind to other biological molecules. Having bound to DNA and proteins, these metabolites form the so-called carcinogen adducts. During a cell division, the presence of such a complex in a DNA region can lead to an incorrect transcription of genetic information, thereby giving a rise to mutation.
The enzymes of phase II biotransformation, which attach the peptide glutathione to the water-soluble metabolites of carcinogens, hinder this process. Eventually, it is as such conjugates that carcinogens are removed from the cell and from the body. The physiological mechanism that restores the normal sequence of nucleotide bases in DNA in case of mutation is DNA repair, implemented with the help of specialized enzymes. However, when the enzyme activity is low, mutations accumulate at each cell division, which may finally lead to malignant transformation of a normal cell.
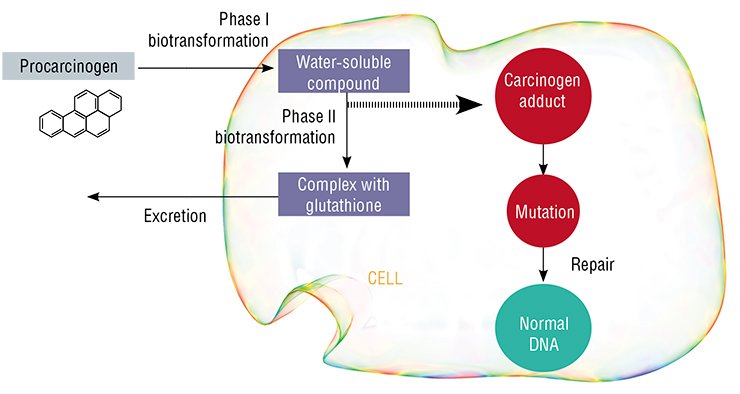
Note that the genes coding for the enzymes involved in biotransformation and repair display a considerable variation (polymorphism). Some variants provide for thesynthesis of active enzyme species; others determine weakly active forms; in some cases the enzyme activity can stop. It is evident that the mutations in DNA can be retained and fixed only when the high activity of the phase I enzymes is combined with the low activity of phase II biotransformation and repair enzymes.
Luckily, such “fatal” combinations are rather infrequent, since each of these three groups of enzymes is encoded by a large number of genes and each gene can have several variants. This is also confirmed by a relatively low rate of cancer diseases in human populations.
There is an immune response!
It is widely believed that one of the causes underlying development of cancer diseases is immune suppression, which can be also caused by chemical carcinogens. However, this is not completely true: being low molecular weight compounds, chemical carcinogens, cannot by themselves induce any specific immune response (synthesis of antibodies); this can be done only by macromolecules such as proteins and peptides.
However, antibodies to chemical carcinogens have been found in the blood serum of both healthy persons and cancer patients, these antibodies being more frequent and numerous in the latter cohort. This raises the following relevant questions: How can chemical carcinogens induce a specific immune response? What is the role of these antibodies in carcinogenesis per se?
The majority of researchers believe that the antigen inducing immune response in this case are the above mentioned adducts, complexes of chemical carcinogens with biomolecules. There is also the concept of immunochemical homeostasis, which implies that the specific antibodies produced in the body bind these carcinogens, thereby decreasing the biotransformation activity (Kovalev and Shipulina, 1992).
However, model experiments have demonstrated that only the antibodies that penetrate from the blood to the lumens of hollow body organs (bronchi and gastrointestinal tract) are able to play such a protective role. On the contrary, in the blood they create an additional gradient for carcinogens, increasing their transport from environment through the epithelium and thereby stimulating carcinogenesis (Silbart et al., 1997; De Buck et al., 2005). The only experiment involving the whole mouse organism demonstrated that benzopyrene induced earlier tumor development in the individuals with a high level of specific serum antibodies (Curtiset et al., 1978).
Scientists from the Institute of Human Ecology tackled the question of what was the correlation between the production of specific antibodies in humans and the operation of their system of chemical carcinogen biotransformation. These studies were necessary for developing a new field in cancer immunoprophylaxis, namely, the designing of anticarcinogenic vaccines.
A double-edged sword
The studies of Kemerovo scientists have demonstrated that lung cancer patients far more frequently display elevated levels of antibodies to the carcinogen benzopyrene as compared with healthy persons as well as higher levels of antibodies to estradiol, a steroid hormone produced in the body. Note that the probability of tumor onset depends on the ratio of these two characteristics. Although the biological meaning of this phenomenon is yet vague, concurrent tests for the antibodies to both the carcinogen and estradiol can be recommended to estimate an individual risk of lung cancer development.
One more pattern was discovered when researchers studied the genetic polymorphism of the enzymes involved in biotransformation of low molecular weight compounds. A correlation between the level of protective antibodies and the gene GSTT1 that encodes an enzyme of phase II biotransformation has been observed in the cohort of lung cancer patients. A mutation in this gene completely deprives the enzyme of the ability to bind active chemical carcinogen species to glutathione.
It is widely accepted that the inactive form of this gene is associated with a high risk of cancer diseases. However, the level of antibodies to benzopyrene in this case was higher in the patients with a functionally active GSTT1 gene. This testifies to the fact that antibody synthesis is induced by the products of phase II biotransformation rather than by the products of phase I, as was assumed earlier.
Presumably, the serum antibodies, forming complexes with protein conjugates of carcinogens, interfere with their penetration from the bloodstream into organs and tissues. Such circulating complexes are taken up by the liver, where they are inactivated. It means that production of antibodies to low molecular weight compounds is a specialized component of the immunological adaptation of humans to the factors potentially hazardous for the cellular DNA.
However, under certain conditions the antibodies to carcinogens are able to boost a genotoxic effect of the latter, thereby inducing carcinogenesis, which has been proved by the study of the chromosome aberrations in the peripheral blood lymphocytes conducted with healthy men with known levels of antibodies to benzopyrene (Glushkov et al., 2011).
An antibody instead of an antigen
Improved immune assays as well as the advent of adequate models for chemical carcinogenesis have recently raised hopes for creating vaccines against chemical carcinogens, which could be used for cancer immunoprophylaxis. Note that the first attempts of this kind were made as early as the first half of the last century in experiments with mice (Frank and Creech, 1939). The main difficulty in designing anticarcinogenic vaccines is in selecting the appropriate antigen. within the case of an infectious disease an inactivated pathogen, safe for humans, is normally used as such. However, it is impossible to inactivate a chemical carcinogen: a considerable change in the structure of its molecule will give another compound that cannot serve as an antigen; in all other cases, the carcinogen retains its mutagenic properties.
For example, to immune animals American researchers successfully used a polycyclic hydrocarbon, fluoromethylbenzanthracene. (Moolten et al., 1981). Yet although the presence of fluorine decreases the carcinogenic properties of the initial compound, such preparations should not be used in medical practice since there always remains the probability of tumor development.
This problem has been resolved using the so-called anti-idiotypic antibodies which are produced via “double immunization” (Chagnaud et al., 1993). First, rabbits were immunized with the benzopyrene conjugated to albumin; then, the “primary” antibodies obtained from rabbits were used to immunize laboratory mice. Using the hybridoma technolowgy*, the “secondary” monoclonal antibodies were raised in mice to immunize laboratory rats. Amazing though it may seem, but despite the fact that these antibodies completely lacked the initial carcinogen, they acted similarly to an anticarcinogenic vaccine, slowing down tumor development upon the impact of benzopyrene. Thus, it was demonstrated that a protective immune response to the carcinogen can be induced with the help of safe protein preparations mimicking the antigenic properties of a carcinogen.
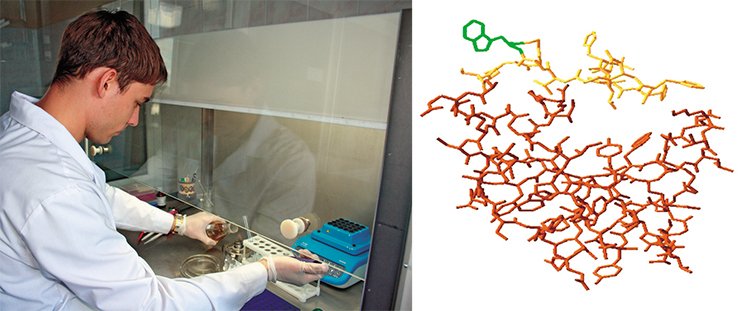
Currently, there are more perfect methods for producing such vaccines. In particular, the so-called phage display was used for this purpose at the Institute of Human Ecology, the method itself ptotected by two patents of the Russian Federation.
At the first stage, Kemerovo researchers synthesized a protein (bovine serum albumin) conjugate with benzopyrene. Then using the hybridoma technology a clone of lymphocytes, cells synthesizing antibodies to benzopyrene, was isolated from the liver of the mice immunized with the conjugate. As has been shown, these antibodies are also able to react with other poly- and heterocyclic hydrocarbons but do not bind the amino acids containing an aromatic ring as well as steroid hormones. This is their advantage in comparison with the known foreign analogs.
At the third stage, five clones able to selectively bind the produced monoclonal antibodies were isolated from a large library of bacteriophages, bacterial viruses widely used in research practice. This means that these bacteriophages contain within their envelope a peptide that is a kind of “protein analog” of benzopyrene. Correspondingly, immunization of mice with one of these clones will induce the antibodies specific to this carcinogen, which is actually required from an anticarcinogenic vaccine (Glushkov et al., 2010)
Тhus, the research results of Kemerovo scientists have confirmed the possibility of designing vaccines for cancer prevention which involve the peptides mimicking immunological properties of chemical carcinogens.
For the first time it was demonstrated that the antibodies to chemical carcinogens in the human body can both resist the genotoxic impact of carcinogens and, on the contrary, increase it, thereby enhancing development of malignant tumors. These results should be taken into account when applying the already known tools for cancer immunoprophylaxis and when developing the new ones. Since the effect of immunostimulation of carcinogenesis cannot be excluded, the widely advertized preparations for “immunity improvement” should be applied with caution.
As for Kuzbass, it is evident that doubling the coal production planned in this region will, with a high probability, lead to an increase in the carcinogenic load on population as well as in cancer morbidity. Therefore, it is most important to limit by any means, including the novel technologies elaborated by the Siberian Branch of the Russian Academy of Sciences, an increase in the volume of industrial discharge.
In addition, it is necessary to develop and apply (first and foremost, at the facilities of heavy and fuel industries) a set of laboratory methods for assessing individual resistance/sensitivity to carcinogenic factors characteristic of Kuzbass, since certain population cohorts are still susceptible to cancer diseases even if the carcinogenic load is low.
References
Glushkov A. N., Larin S. A. i dr. Zabolevaemost’ zlokachestvennymi novoobrazovanijami v Kemerovskom AO “KOKS”// Voprosy onkologii. 2005. T. 51, № 4. S. 444—446.
Glushkov A. N., Apal’ko S. V. i dr. Monoklonal’nye antitela k himicheskim kancerogenam gruppy policiklicheskih aromaticheskih uglevodorodov// Rossijskij immunologicheskij zhurnal. 2009. № 3. S. 30—38.
Ocenka i prognoz kancerogennoj opasnosti dlja naselenija ugledobyvajushhih regionov Rossii i Ukrainy (na primere Kemerovskoj i Doneckoj oblastej) / pod obshh. red. A. N. Glushkov, G. V. Bondar’; Ros. akad. nauk, Sibirskoe otd., In-t jekologii cheloveka [i dr.] // Novosibirsk: Izd-vo SO RAN. 2010. 156 s.
Glushkov A. N., Apalko S. V., et al. A Novel Approach to the Development of Anticarcinogenic Vaccines // Acta Naturae. 2010. V. 2. No. 4 (7). P. 105—111.
* Hybridomas, the cells produced by fusing lymphocytes and tumor cells, are able to synthesize specific antibodies as well as to continuously grow in cell culture