Atherosclerosis: A Tender Killer. From Theory to Practice
Cardiovascular diseases are justly called an epidemic of the 20th century: during the last decades, they became the main cause of increased mortality level in the industrially developed countries including Russia, being responsible for about 1,200,000 deaths annually. Unfortunately, the situation at the beginning of the new century has not virtually changed: the cardiovascular “epidemic” continues to gather its plentiful harvest
The mortality rate from cardiovascular diseases (CVD) in Russia today is two — fourfold higher as compared with the Western European countries, USA, Canada, and Australia and, unfortunately, it still displays a trend for growth. On the contrary, a decrease in the CVD mortality is recorded in many developed countries over the last 30 years. First and foremost, this phenomenon is connected with the changes in life style, namely, cessation of smoking, healthy diet, and higher physical activity.
The term atherosclerosis was proposed by German pathologist F. Marschan in 1904 to define the disease in which arterial sclerosis was determined by the abnormalities in lipid (fat) and protein metabolisms. The word atherosclerosis is composed of two Greek roots — ather (chaff) and sclerosis (hardening). These words polar in their meanings precisely reflect the pathological processes characteristic of this disease, namely, accumulation of soft deposits, overgrowth of connective tissue, and calcification, which makes arteries dense and rigid.
Usually heart ischemia, stroke, and the involvement of peripheral arteries are ascribed to CVD, as they have common risk factors, although the significance of particular factors can be different. Note that the leading role in development of these diseases is assigned to atherosclerosis, a chronic disease causing changes in the walls of blood vessels and impairing their functions, which leads to an insufficient oxygen supply to the tissues and organs (ischemia). What is the cause of this threatening disease and is it possible to struggle with this merciless “tender killer”?
Yellow, White, and Vulnerable
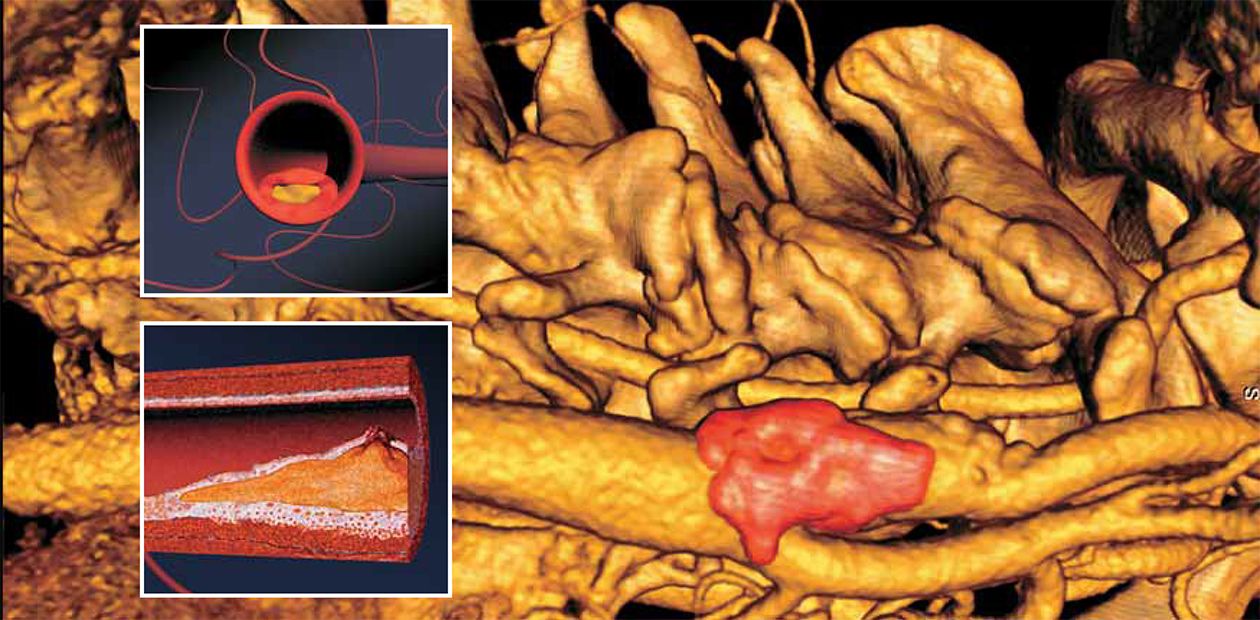
The morphological “carrier” of atherosclerosis is the so-called atherosclerotic plaques — dense oval or round-shaped structures colored white or yellowish white, which rise above the surface of vessel internal tunics and narrow their lumen. The fibrous plaques are most frequently detected in the abdominal aorta and its outgoing branches as well as in the carotid arteries and arteries of the heart, brain, kidneys, lower extremities, and so on.
At the early stages, the plaque is a thin capsule of connective tissues containing large amounts of lipids. This is the so-called yellow or vulnerable plaque. The latter name is very exact, as the thin envelope of these plaques can be damaged by both hemodynamic factors (a pressure change in the vessel) and specialized proteins produced by the cells of the immune system in the neighborhood of the capsule membrane.
When an atherosclerotic plaque is ruptured, the biologically active substances secreted by platelets can lead to a spasm of the coronary artery; this induces the development of unstable angina pectoris (focal myocardial infarction with a mural thrombosis of the coronary artery) or large-focal myocardial infarction, with a possible sudden lethal outcome. Necrosis of deep blood vessel layers can lead to development of aneurysm (a protrusion of the wall), which can later be ruptured, also causing sudden death.
The fatty substances released from the ruptured capsule contact platelets, a type of blood cells, resulting in an immediate formation of a thrombus. In addition, the biologically active substances secreted by platelets can cause a spasm of the coronary artery. This induces the acute coronary syndrome — an unstable angina pectoris or myocardial infarction — leading in some cases to a sudden death.
A necrosis of deep blood vessel layers can lead to the development of aneurysm, a protrusion of the wall. Frequently, the blood detaches the internal tunic of the vessel from its middle tunic, forming the so-called dissecting aneurysms. Such complications are fraught with the risk of rupture of either the aneurysm itself or a cell wall.
At the late stages, the fibrous plaques become dense structures with a firm connective tissue capsule and relatively low lipid content; they are called white plaques. Causing a pronounced (by 75 % and more) narrowing of the coronary artery, the plaques thereby are the morphological substrate of a stable exertional angina pectoris. A rupture of the firm fibrous capsule cannot be excluded too; however, this is more likely for the yellow plaques.
The final stage of atherosclerosis is atherocalcinosis, characteristic of which is calcification, i. e., the deposition of calcium salts into fibrous plaques.
Thus, atherosclerosis can have both acute and chronic complications. Protruding into the lumen of a blood vessel, the atherosclerotic plaque contributes to the narrowing (stenosis) of the lumen (stenotic atherosclerosis). As plaque development is rather slow, a chronic ischemia is formed in the blood supply region of the affected vessel. The chronic circulation deficiency is accompanied by anoxia, dystrophic and atrophic changes in the corresponding organ, and overgrowth of the connective tissue.
The acute complications of atherosclerosis are determined by the angiospasm and formation of thrombi and other occluding bodies, emboli. The vascular occlusion accompanied by acute circulation deficiency (acute ischemia) leads to development of the infarctions of various organs, such as myocardial infarction, limb gangrene, and others. Sometimes, the rupture of aneurysm can have a lethal outcome.
Cholesterol Is to Blame?
The theory is now popular that regards atherosclerosis as the response to the damage of vascular walls with cholesterol, a fat-soluble steroid substance present in all the tissues of animal body, as the key injurious factor.
It was discovered at the end of the last century that the concentration of cholesterol is doubled in the regions of atherosclerotic lesions of the vascular wall as compared to the healthy regions. As was shown experimentally, addition of this substance to rabbit diet results in the development of aorta lesions resembling the atherosclerotic changes in human vessels.
Thus, the infiltration theory of atherosclerosis was formulated. In essence, it is considered that the key point in the development of this disease is cholesterol infiltration into the internal tunic of arteries (lipidosis) with the subsequent overgrowth of connective tissue (sclerosis).
Cholesterol circulates in the blood as protein—lipid complexes containing triglycerides, phospholipids, and proteins. Two main classes of cholesterol carriers — the so-called low density lipoproteins (LDL) and high density lipoproteins (HDL) — perform different functions. The former interact with the specific receptors in the cell membranes, providing the transport of cholesterol to the cells of peripheral tissues. On the contrary, the latter are able to “take away” the excess cholesterol when contacting the cell membranes and transport it back to the liver, where it is degraded to form bile acids.
The concentration of low density lipids and their lifespan in the blood of atherosclerosis patients increase; moreover, some of these lipoproteins are subject to peroxidation, which renders them especially dangerous. The latter lipoproteins are able to injure directly the endothelium of vascular walls and interact with blood clotting factors, enhancing thrombus formation.
These data are confirmed by numerous epidemiological studies, which have demonstrated that the level of cholesterol in high density lipids is inversely proportional to the presence of heart ischemia, which can be used for assessing the risk of ischemia development.
As great importance is attached to the role of early (vulnerable) plaques in the development of acute coronary syndrome, prevention of their development may be regarded as the main goal in treatment of primary heart ischemia and, especially, prevention of the secondary one. The therapy with statins, the drugs decreasing the cholesterol level in blood, can stabilize the atherosclerotic plaque, i. e., strengthen its capsule and decrease the likelihood of its rupture.
The experience in applying such preparations demonstrates that the favorable effect in many patients is observed already during the first weeks of treatment, when the regression of atherosclerotic lesions is yet out of question. First and foremost, this is connected with the fact that a decrease in the cholesterol level in blood ameliorates the vessel functioning, normalizes the blood clotting system, and restores the generation of nitric oxide (NO) suppressed during hypercholesterolemia. The decrease in the cholesterol level in blood allows for restoring the ability of arteries to dilate under the action of biologically active substances.
Two Hypotheses
The hypothesis that inflammation and infection are involved in the development of atherosclerosis was proposed as early as in the 1990s, and the volume of data confirming it is steadily increasing. It is proved that a local inflammation in the cells of medium and large arteries is a specific immune response (activation of T lymphocytes) accompanied by a nonspecific increase in the number of monocytes — a type of leukocytes (the blood cells capable of phagocytizing and involved in the inflammatory reactions) — in the arterial wall.
Electron microscopy has detected macrophages — relatively large blood cells capable of capturing and digesting foreign or toxic objects — between vascular cells (at the sites of future sclerotic plaques) which migrate to the vessel lumen and back. The accumulation of macrophages is an early morphological sign of the disease. The molecular mechanisms providing adhesion of macrophages to the inner surface of vessels are similar to those observed during an acute inflammation. Presumably, this is one of the early molecular mechanisms of plaque formation.
The formations composed of macrophages, lymphocytes, and smooth muscle cells encompassed usually by fibrous tissue are among a large number of developing atherosclerotic plaques. Platelets cluster around a plaque, which is accompanied by a damage of vascular cells. All such interactions between blood cells and vascular endothelium are now being actively studied.
The liver cells during both inflammation and atherosclerosis intensify the synthesis of special inflammatory proteins (C-reactive protein, lipoprotein, and fibrinogen) and their secretion into the blood. Clinically, the inflammatory syndrome and sclerotic process can go on for a long period with alternation of exacerbations and remissions, i. e., both processes comprise the same functional reactions. That is why it is considered that elevated levels of fibrinogen and C-reactive protein in combination with increased erythrocyte sedimentation rate indicate the risk of cardiovascular diseases.
The discovery of microorganisms, such as Helicobacter pylori, Chlamydia pneumoniae, and some others, in the atherosclerotic plaque and blood is a confirmation of the infectious theory of atherosclerosis. Developing further the hypothesis on an infectious etiology of atherosclerosis, Italian scientists proposed a connection between heart ischemia and hepatitis C virus.
It is now accepted that the impairment of nitric oxide synthesis plays the key role in the development of endothelial dysfunction and, possibly, atherosclerosis. It is believed that NO is the particular agent that makes blood vessels relax in response to an external stimulus. (At least, the use of L-arginine, a substrate for NO generation, in the therapy of atherosclerosis results in amelioration of the vessel functioning.) A decreased NO level in the vicinity of atherosclerotic plaques enhances a persistent vascular spasm in the region of atherosclerotic lesion.
Interestingly, an impaired vessel relaxation is recorded not only in atherosclerosis patients, but also in the individuals with the propensity for this disease and smokers.
Inherited Atherosclerosis
Many researchers have analyzed the significance of hereditary factors in the development of atherosclerosis. There is ample evidence that the family members belonging to the same surname lineage display similar negative shifts in their fat metabolism; correspondingly, the risk to develop atherosclerosis for them is higher than for those lacking blood ties. In addition, close relatives display similar location patterns of atherosclerotic lesions in the coronary or brain vessels. It has been also demonstrated by a more detailed examination that young healthy individuals with compromised inheritance display a pronounced trend for increase in the cholesterol level as well as certain other metabolic changes indicating atherosclerotic processes.
Anyway, what is the mechanism that realizes such family hereditary predispositions to atherosclerosis? It is evident that the type of response of the organism to environmental factors is the trait that is inherited. It may be assumed that the reason lies in rapid changes in the living conditions of the contemporary man and the overstrain of the adaptive systems, in particular, nervous, endocrine and cardiovascular systems, which impairs their function leading thereby to the development of atherosclerosis.
The correlation between the mutation frequency of certain genes controlling antisclerotic inflammatory lipoproteins and nitric oxide, on the one hand, and the probability of atherosclerosis development of various localizations, on the other, has been established. In particular, the individuals carrying a number of mutations in the gene coding for endothelial NO synthase more frequently get angina pectoris, myocardial infarction, and arterial hypertension as compared with other individuals.
The patients carrying various mutations in the genes involved in the system of blood hemostasis more frequently develop thrombosis on the background of atherosclerosis complications, which suggests that the detection and study of gene polymorphisms in atherosclerosis cases is a very promising direction. In particular, the Department of New Medical Technologies with the Institute of Chemical Biology and Fundamental Medicine, which is involved in the research into basic aspects of atherosclerosis, has accumulated data on frequently occurring mutations in the gene system controlling thrombus formation. Also, it has been discovered that the risk of cardiovascular diseases is higher in the individuals carrying one of the alleles of gene APOE (allele E4), encoding the protein component of certain plasma lipoproteins. The carriers of this gene isoform display increased levels of both total and LDL cholesterol, which fits well the data available in the medical literature.
A complex examination, including genetic tests (detection of mutations in the apolipoproteins and the system regulating nitric oxide generation), makes it possible now to develop individual treatment schemes for the patients with different atherosclerosis manifestations aiming to provide a timely and differential correction of this pathological state at the earliest stages of its development.
Those Who Risk
Even though the term atherosclerosis was proposed over one hundred years ago and the disease itself has been studied actively, the question about its causes and risk factors still has no final answer.
Over 30 factors the action of which increases the risk of atherosclerosis onset and development are known now. All these factors can be conditionally divided into two groups: the factors that cannot be changed by human will (for example, age) and modified factors, such as smoking.
The age influences directly the rate and severity of atherosclerosis. This is in no way surprising: the main metabolic processes (lipid, carbohydrate, and vitamin), immunological activity, function of the liver, etc., change with age, potentially enhancing the disease development. However, numerous data demonstrate that this disease can commence in early adolescence! A large-scale examination of donor hearts aged 13—19 years detected the signs of atherosclerosis in approximately each sixths and over 70 % displayed at least one atherosclerotic lesion by the age of 40.
Nonetheless, it is evident that the age itself cannot be regarded as the cause of atherosclerosis. After all, many elderly persons living under the same conditions as atherosclerosis patients display no signs of this disease. There are also pathomorphological data demonstrating the absence of atherosclerotic lesions in the blood vessels of very old people. All these exceptions refute the fatality of age factor in the development of atherosclerosis.
Sex also influences the likelihood of atherosclerosis: the atherosclerosis morbidity rate at an age of 50—60 years is higher in men than in women. This fact attracted attention of researchers to the role of sex hormones in the pathogenesis of atherosclerosis. They succeeded in obtaining many data demonstrating that female sex hormones, estrogens, delay the development of atherosclerosis (this is connected with an increase in the content of high density lipoproteins in the blood plasma, which, as is mentioned above, have an antisclerotic effect). During the menopause, the level of estrogens in women decreases, which is accompanied by the growth in the level of cholesterol, the cholesterol-to-phospholipids ratio, and the cholesterol of low density lipoproteins in the blood serum, thereby elevating the risk of atherosclerosis development.
One of the most significant risk factors for atherosclerosis is obesity. However, it is appropriate to quote here an observation of US researchers made based on a mass examination of the myocardial infarction cases in the USA: half of the patients had an excess weight; one-forth displayed a reduced weight, and only each fourth was obese. Consequently, not the obesity itself is important but rather the increased level of lipids in the blood and arterial pressure, frequently accompanying obesity, as well as other adverse factors, such as genetic load, overeating, and sedentary life style.
As for arterial hypertension, it unambiguously influences the onset and progress of atherosclerosis, because hypertension is accompanied by many adverse changes, including an elevation in the vascular wall permeability, thickening of inner tunic of arteries, increase in the arterial wall rigidity, propensity for spastic constrictions, as well as a trend for the development of thrombosis.
Another essential risk factor for atherosclerosis is diabetes mellitus, because carbohydrate and lipid metabolisms are to a certain degree interconnected. It is found that the insulin sensitivity of peripheral tissues, mainly, adipose tissue, during both atherosclerosis and diabetes mellitus decreases.
Nonetheless, many scientists regard psychoemotional stress as the most important risk factor for atherosclerosis, as has been demonstrated in both animal models and humans. Today we can speak about the so-called unresolved emotional reaction, i. e., the state when psychoemotional conflicts are not finalized (fail to end as a particular physical event). This enhances accumulation of the substances that are induced by stress (lipoproteins, catecholamines, etc.), which trigger the atherosclerotic process.
That is why people who go in for sports or whose occupation is connected with physical activity get atherosclerosis or the diseases developing as its consequence (angina pectoris, myocardial infarction, and stroke) considerably rarer even on the background of high emotional stress. The blood of those leading an active life contains an elevated level of high density lipoproteins, which protects them from development of atherosclerosis.
Thus, the progressive spread of atherosclerosis all over the world is a consequence of distorted natural needs of human as a biological being, the pay for unwise use of the fruits of civilization. High rate of activities, unhealthy way of living, emotional and psychic stresses of modern people are the factors enhancing the epidemiological growth in atherosclerosis, continuing in the new century.
Indeed, we cannot put back the clock and regain our youth, nor are we able to change our inheritance. However, any of us can help himself/herself by changing his/her own life and way of thinking and, with the assistance of a cardiologist, part with the medical problems that are already subject to correction.