Tick-Borne Borreliosis: A Life-Long Disease?
In Russia, borreliosis (or Lyme disease, as it is called in the USA) was first detected serologically (that is, according to the presence of specific antibodies) by the research team of the Gamaleya Institute of Epidemiology and Microbiology with the Russian Academy of Medical Sciences guided by E. I. Korenberg as early as in 1985. However, the ixodid tick-borne borreliosis (ITBB) was included into the official state list of the diseases recorded on the territory of Russia only in 1991.
Tick-borne encephalitis, a dangerous viral disease affecting the central nervous system, hardly needs any introduction, especially, in connection with the recent seasonal peak of morbidity. However, another disease, now of bacterial origin, and also borne by ticks has attracted the attention of Russian physicians and scientists only recently
In Russia, borreliosis (or Lyme disease, as it is called in the USA) was first detected serologically (that is, according to the presence of specific antibodies) by the research team of the Gamaleya Institute of Epidemiology and Microbiology with the Russian Academy of Medical Sciences guided by E. I. Korenberg as early as in 1985. However, the ixodid tick-borne borreliosis (ITBB) was included into the official state list of the diseases recorded on the territory of Russia only in 1991.
This illness is most widespread in the USA, where over 16,000 borreliosis cases are recorded annually. The growth in borreliosis morbidity rate is now also observed in many European countries.
Spirochete is the Causative Agent
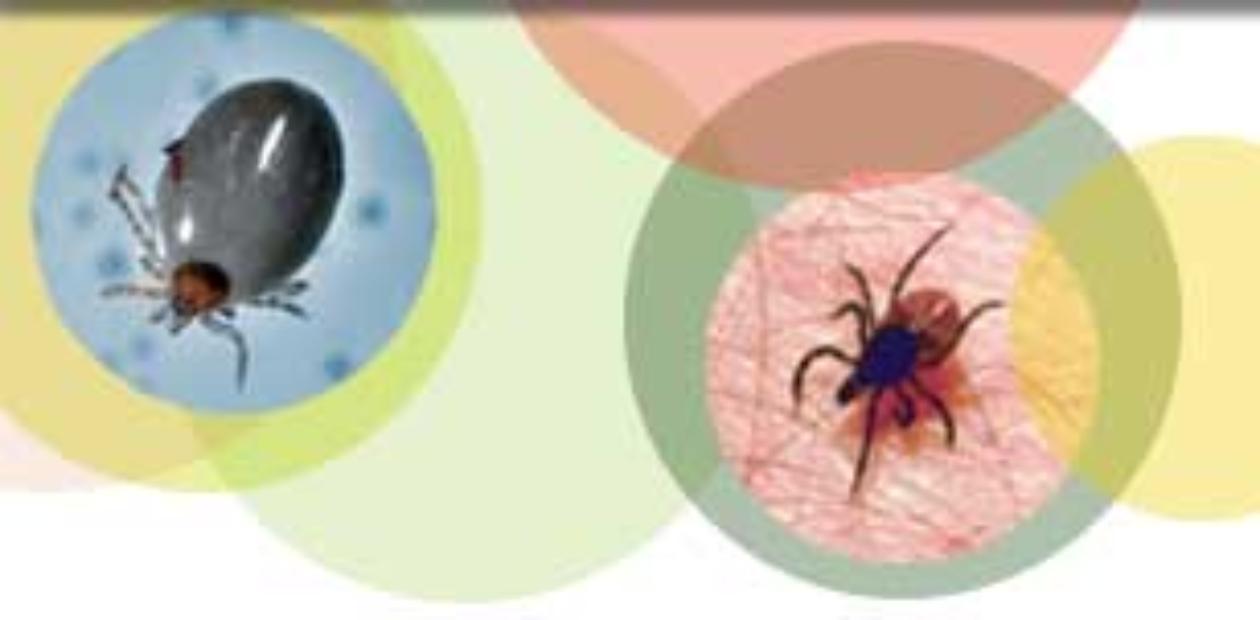
The name of this illness itself makes it evident that ticks, as in the case of tick-borne encephalitis, are its vectors. In the USA, the disease is transmitted by the ticks Ixodes scapularis (Willy Burgdorfer, an American researcher, isolated the corresponding infectious agent from these particular ticks), and the carriers in Europe are another tick species, Ixodes ricinus. As for this country, the notorious taiga ticks Ixodes persulcatus play this role.
The causative agent of borreliosis, a spirochete from the complex bearing a splendid name of Borrelia burgdorferi sensu lato (s. l.), is a close relative of treponema, the pathogen causing the well-known syphilis, and leptospira, the agent of leptospirosis, a severe disease affecting many animal species, including humans. All the mentioned spirochetes have similar appearance and their shape resembl a coiled helix.
Borrelia are not only capable of migrating under the skin, but also of penetrating into the blood vessels, where they travel to the internal organs with the blood flow. The blood–brain barrier, which protects brain blood vessels, is not an obstacle for them
So far 12 borrelia species have been described based on genetic and phenotypic distinctions, and only three of them — B. burgdorferi sensu stricto (s. s.), B. afzelii, and B. garinii — were considered dangerous for humans. However, as was reported recently, one more species, B. spielmanii, was isolated from borreliosis patients, which suggests the potential pathogenicity of this species as well.
Borrelia are spread unevenly all over the world. Two species — B. afzelii and B. garinii — are of the main epidemiological importance in Russia. These species are found in the vast forest zone from Baltic countries to Southern Sakhalin.
Research into borrelia was commenced at the Institute of Chemical Biology and Fundamental Medicine in the year 2000. The studies conducted in collaboration with the Institute of Animal Systematics and Ecology, Siberian Branch of the Russian Academy of Sciences, aimed to detect the species diversity of borrelia that circulate in the ITBB natural foci of the Novosibirsk oblast, have clarified a number of facts. In addition to the widespread B. afzelii and B. garinii, some rarely occurring genetic variants of these species have also been found.
According to the microscopy data, the rate of borrelia in the taiga ticks on the territory of the Novosibirsk oblast amounts to 12—25 %. Moreover, microscopic examination of both fixed and intravital preparations detects borrelia in adult ticks, collected from plants, as well as in partially or completely fed larvae and nymphs.
These spirochetes were found at all the stages of tick development, from larvae to adult individuals (imago), which means that any stage is a source of infection. The cycle of pathogen transmission commences from the feeding of an uninfected tick on an infected animal. The ticks infected with borrelia are able to transmit these microorganisms to healthy animals during the next feeding or to receive an additional portion of spirochetes from infected mammals. Small mammals are involved in this process at the early stages of tick development, whereas adult ticks feed on large mammals and can “attack” and infect humans.
Invading the body of a mammal with the tick saliva, spirochetes start to reproduce in the skin at the site of the biting. They are not only capable of migrating under the skin, but also of penetrating into the blood vessels, where they travel to the internal organs with the blood flow. The blood — brain barrier is not an obstacle for them, and reproducing in the cerebrospinal fluid, they cause severe neuroinfections.
The First Stage is Reversible
Ixodid tick-borne borreliosis is a multisystem disease that can cause skin lesions and affect the musculoskeletal, nervous, and cardiovascular systems. The pattern of clinical manifestations of this disease depends on its stage. Three stages of borreliosis infection are conditionally defined, although they are not always distinctly distinguishable. As a rule, borreliosis develops successively, passing from one stage to another.
The first stage lasts from 3 to 30 days. During this period, a red ring may develop on the skin (at the site of the tick bite) due to the development of inflammatory reaction, which has a corresponding name, circular migrating erythema. It starts from a small spot at the site of the bite and migrates to the periphery. In typical cases, the center of this spot lightens, whereas the periphery forms a red elevation with a shape of an irregular ring with a diameter of up to 15 cm.
Examination of the skin sampled from various parts of the erythema demonstrates the virtual absence of borrelia in the center of this ring and typical presence in the periphery. The erythema can remain on the skin much longer than other inflammatory changes.
In addition to skin manifestations, approximately one-fourth of the patients also develop the following symptoms: chill, drowse, muscle weakness, joint pains, and enlarged lymph nodes. This indicates that borrelia are spreading over the organism. However, the early stages of borreliosis are not accompanied by intoxication symptoms in the majority of the patients with developed erythema. Moreover, there is the so-called erythema-free form, which, as a rule, starts as an acute process complicated with fever, joint pains, and headache.
Treatment of the last, third stage of borreliosis, which develops half a year — a year after the infection, requires a long-term antibiotic therapy. Struggle with the chronic disease is not always successful
Note also that the absence of the symptoms during the first period after the bite of the tick in no way guarantees that the disease would not develop in future. However, a timely treatment at the first stage can provide a complete recovery.
The second stage of borreliosis develops on the average 1—3 months after the infection. By that time, borrelia migrate with the blood and lymph flows to various organs and tissues, including the muscles, joints, myocardium, spinal cord, and brain as well as the spleen, liver, and retina, and affects them. That is why a considerable diversity of clinical manifestations — neurological, cardiac, dermal, and others — is characteristic of this stage.
The involvement of the nervous system appears as meningitis, mono- and polyneuritis (most frequently, facial neuritis), and other disorders. Many of these symptoms may appear simultaneously. The most frequent neurological manifestation is perhaps meningoradiculoneuritis (Bannawarth syndrome), with a characteristic facial nerve paresis. Besides, secondary erythema may develop in certain cases at this stage of disease.
The last, third stage of borreliosis develops half a year — a year after the infection had entered the body. The most frequent cases include involvement of joints (chronic arthritis), skin (atrophic acrodermatitis), and chronic affection of the nervous system (chronic neuroborreliosis). The late stage of borreliosis requires a long-term antibacterial therapy; nonetheless, some arthritis patients still retain the signs of chronic infection for months and even years after treatment with antibiotics has been completed.
The Immune Response
As a rule, several pathogenic mechanisms are involved in the development of borrelia infection. Some syndromes, such as meningitis and radiculitis, are likely to reflect the result of the direct infection of the corresponding organ, whereas arthritis and polyneuritis may be connected with indirect effects caused by the secondary autoimmune responses.
The immune response of the body to borrelia infection manifests itself differently. To control the spreading of infection, the organism uses both the innate immunity (nonspecific resistance) and the adaptive specific immune response, i. e., the production of specific antibodies to a particular infectious agent. During the first two weeks after the onset of the disease, the immunoglobulins against certain borrelia antigens — the infectious proteins that trigger the mechanism of immune response in the body — are actually found in the majority of borreliosis patients.
As early as in the 1990s, the first studies into the development of vaccine against borreliosis were conducted in the USA. Nonetheless, no efficient vaccine that would prevent this dangerous disease is available yet. Presumably, the difficulties encountered when developing safe vaccines are connected with the specific features of the immune response observed during borrelia infection. In the case of this disease, the immune response can induce production of the antibodies to certain proteins of the body, i. e., cause harmful autoimmune reactions.
The reason underlying such immune response is molecular mimicry, or similarity. For example, the borrelia lipoprotein OspA is similar to the adhesion protein hLFA-1a, which is produced by our T cells in the synovial membrane, lining inner surfaces of the joints. Correspondingly, the complications that developed after immunization with the vaccine involving lipoprotein OspA in the majority of cases appeared as arthritis and autoimmune rheumatoid arthritis. The work on creation of an appropriate and safe yet efficient vaccine is still in progress.
How to diagnose ITBB
ITBB is usually diagnosed based on the so-called epidemiological anamnesis (the fact of visiting a forest and the bite of tick) and clinical signs of a disease, the presence of migrating erythema being the main one.
The cases proceeding in an erythema-free variant of the disease concurrently with other tick-born infections, for example, tick-borne encephalitis or anaplasmosis, are especially difficult to diagnose.There have been clinical cases when erythema-free borreliosis and tick-borne encephalitis were simultaneously found in a patient; as a result, the patient was hospitalized for the second time because of the complications.
Erythema-free cases can be diagnosed only by laboratory tests. Isolation of borrelia from samples of skin, blood serum, cerebrospinal, or synovial fluids and their cultivation on special media require specialized conditions and expensive reagents to say nothing about the long time it takes and how inefficient it is.
The first studies on developing of the vaccine against borreliosis were conducted as early as in the 1990s.
Nonetheless, no efficient vaccine that would prevent this dangerous disease is available yet
Microscopic examination is, as a rule, used when analyzing the infection of ticks with borrelia but actually is not applicable to ITBB diagnostics, as borrelia never accumulate in human tissues in the amounts detectable by microscopy.
Borrelia can be detected by polymerase chain reaction (PCR), which allows the DNA of this agent to be recorded. Our PCR-based studies have demonstrated that the number of borrelia per one tick varies from one to six thousand. However, similarly to the other methods, it is not recommended to use the PCR-based test in diagnosing borreliosis independently, as its sensitivity is yet insufficient, which can lead to the so-called false negative results.
Nonetheless, our joint work with the Municipal Infections Hospital no. 1 (Novosibirsk) has demonstrated that this method is quite appropriate in combination with immunological tests at the early stage of disease before treatment.
The detection of DNA during the first four weeks after the tick bite can provide a timely detection of the mixed infection. However, a negative test does not exclude the infection; thus, serological tests (for detection of specific antibodies) should by made 3—6 weeks later.
The detection of antibodies to borrelia proteins is presently the main method of laboratory diagnostics. To elevate the reliability of serodiagnostics, a two-level system for testing blood sera is recommended and used in the USA and in European countries. However, the two-level approach has not been used in Russia due to the absence of domestic test kits. In addition, the immunoglobulins from the blood serum of ITBB patients can react differently to the main proteins of different borrelia species. Therefore, the testing criteria developed for one country can be inappropriate for another.
In Russia, serological detection methods with comparable diagnostic values are widely used now; namely, enzyme immunoassay (EIA) and indirect immunofluorescence reaction (IIFR). However, the applicability of the latter is limited due to possible cross-reactions with closely related microorganisms, in particular, Treponema palladium, the agent of syphilis. All in all, even if we use the combination of the state-of-the-art serological tests, the efficacy of antibody detection in patients depends on the disease stage.
Thus, what is borreliosis? Is it a common infection or a lifelong disease? Actually, this illness is not as harmless as it seems at first glance. Sometimes borrelia infection causes severe remote sequelae and diseaseswhich can be attributed to previous borreliosis only after a close examination.
A favorable outcome of this serious bacterial disease transmitted by ticks in many respects depends on the timely and adequate diagnosis and therapy. Note that the treatment of ITBB must not be reduced to thoughtless taking of antibiotics, as it sometimes occurs. This is the work for professionals who are able to clarify not only the clinical symptoms, but also individual specific features of the disease course and occurrence of the concomitant diseases.