The Time of Bloodless Surgery
The new century is a bonanza period for surgery: both the surgical techniques and the approach to surgical intervention are being changed. Surgeons have at their disposal the unique equipment that has drastically changed the technology of surgical intervention, making it less traumatic, safer, and, which is important for patients, more “comfortable”. The modern surgical techniques allow the post-surgery patients to rehabilitate quickly and completely
The tools of modern surgeons in no way resemble the sows and sharp iron hooks of their old-time colleagues. A copper knife, bronze or iron hatchet, and steel lancet are the remote ancestors of the exquisite disposable blades of manifold shapes with laser-sharpened cutting edges. However, even this modern miracle is to make room for new generation tools–laser beam, ultrasound, and radio-frequency radiation. State-of-the-art ultrasonic and radio-frequency scalpels and electric coagulators are not only simple in use, but also gentle in manipulations with the body tissues. Incisions made with such tools take a short time to heal, and the ultimate cosmetic effect is brilliant.
 However, the course of the intervention and post-surgery period are influenced not only by the surgical equipment. The age-long problem in surgery is struggle with pain. In a modern operating room, one will no longer see the classical picture immortalized in movies: the surgeon pours out ether solution drop by drop on the gauze mask covering the patient’s face. Nowadays, anesthesiologists possess almost space-level machinery and a multitude of monitoring systems, which allow them to control the depth of general anesthesia and the patient’s state during the intervention. Unlike their ancestors, the preparations used today for general anesthesia are well tolerable for patients, nontoxic, and are completely excreted from the body in an unchanged form several hours after the surgery.
However, the course of the intervention and post-surgery period are influenced not only by the surgical equipment. The age-long problem in surgery is struggle with pain. In a modern operating room, one will no longer see the classical picture immortalized in movies: the surgeon pours out ether solution drop by drop on the gauze mask covering the patient’s face. Nowadays, anesthesiologists possess almost space-level machinery and a multitude of monitoring systems, which allow them to control the depth of general anesthesia and the patient’s state during the intervention. Unlike their ancestors, the preparations used today for general anesthesia are well tolerable for patients, nontoxic, and are completely excreted from the body in an unchanged form several hours after the surgery.
Of utmost importance for successful surgery is the suture material. For centuries, surgeons used fibers made of natural silk, cotton, and metals; animal (more frequently, sheep) tendons; wooden fibers; and other natural materials (perhaps, the most extraordinary suture material is the ants’ mandibles). However, of this exotic set, only silk and catgut (the self-dissolving cord made of intestinal connective tissues of various cattle) have remained in the present day surgery. As the number and complexity of surgical interventions increased, the requirements to suture material were becoming more stringent. During the last 40 years, diverse synthetic materials–fibers of various structures (smooth, twisted, or braided), often with polymeric covers–have been created. Such materials can stay for a long time in body tissues without the risk of rejection. The wound edges are additionally fastened with a special glue, acting up to 10 days, i. e., until complete healing.
Spare parts for the body
Notwithstanding the availability of the up-to-the-minute suture material and tools, surgical treatment of some diseases requires substitution of the affected organs. First and foremost, this relates to chronic diseases of joints leading to impairments in intra-articular cartilage surfaces. These patients develop the so-called “deflection” of joints, which is accompanied by shortening of the corresponding limb and constant excrutiating pains. However, there is a way out: surgical replacement of worn joints with artificial substitutes made of hi-tech materials (titanium alloys and polymers) has become a routine procedure. Today, endoprosthesizing (this is how the implanting of an artificial joint is called) is able to restore the quality of life even for those over 80 years old.
Dental implants are also made of a titanium alloy. The artificial tooth “root” is a screw placed directly into the jaw bone tissue to replace the lost tooth. The replantation takes about 3 months; then a dental crown is placed onto the implant. Such artificial substitutes are frequently more durable than the natural teeth.
A major problem in stomatology is treatment of bone defects resulting from severe traumas of facial skull or destructive inflammatory diseases. Until recently, healing of these injuries was a difficult and frequently ungrateful task. The advent of plastic bone implants – biocomposites containing collagen and hydroxyapatite (the main components of the intercellular substance of bone tissue), various growth factors, and bone proteins–has changed the situation. This material, placed directly into a defect in the bone tissue, enhances a rapid restoration of the bone’s anatomical shape, and considerably accelerates the healing process and rehabilitation of patients.
Surgical intervention has become frequent for eye diseases. The excimer laser vision correction, which appeared in the 1980s, was a revolution in ophthalmology. Its essence is the removal of defects in the eye optical lens by smoothing the corneal surface with a “cold” laser beam according to an individual computer correction program.
The radiation of a cold laser is also used for a rather unusual treatment of age-related macular dystrophy (the retinal dystrophy caused by a vascular pathology). The function of laser here is in activating the drug visudyne, which, after an intravenous administration, restores the normal physiological processes in the retina and accumulates in the retinal blood vessels of the affected eye.
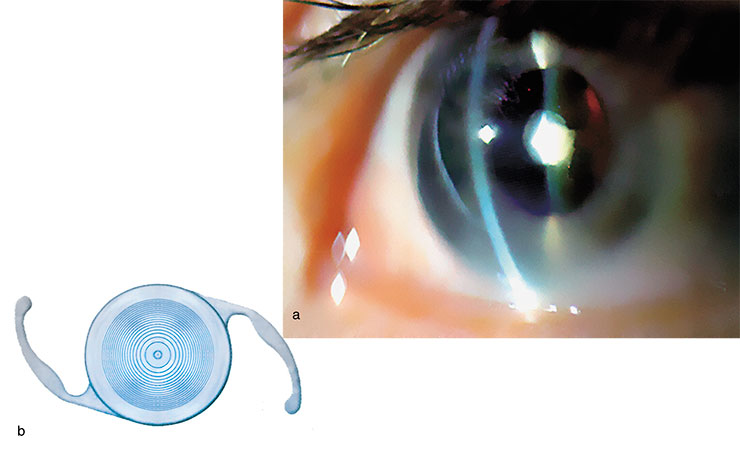
Most patients with a cataract (opacity of the eye lens), which is becoming ever more frequent, also need surgical intervention. For this purpose, they use a phacoemulsification technique with implantation of an artificial intraocular lens. The eye lens is destroyed under local anesthesia with the help of an ultrasonic device through an incision in the eyeball as small as 1.5–3.0 mm. The first intraocular lenses appeared about 60 years ago and were made of a rigid material. In the 1980s, ophthalmologists got at their disposal soft lenses, which could be rolled before being installed into the eye chamber. The up-to-the-minute models of intraocular lenses, bifocal lenses, require no post-surgery vision correction with eyeglasses.
Looking inside
Among the most impressive advances in modern medicine is undoubtedly the adoption of minimally invasive surgery. Since long ago, surgeons have dreamed to directly examine the abdominal cavity, joints, stomach, urine bladder, and bronchi without injuring the patient.
This dream came true in 1901, when D.O. Ott, a Russian gynecologist, performed the first in the history “ventroscopy”, an endoscopic examination of abdominal cavity through small incisions in the anterior abdominal wall. Yet the boundless vistas opened up by the novel surgery became clear only 85 years later, when French surgeons performed a laparoscopic cholecystectomy (surgical removal of the gallbladder). The minimally invasive surgery techniques developed in an avalanche manner, involving, after the abdominal organs, the thoracic cavity, retroperitoneal space, blood vessels, heart, and other organs.
Today, the endoscopic surgery of the abdomen and small pelvis organs is performed through small incisions in the abdominal wall, and the incision sites are determined by the required surgical manipulations. The surgical tools, such as hooks, clamps, and scissors of minute size, are manipulators with the corresponding working heads. Looking at the display, a surgeon does the surgery without touching either the wound or the affected organ. On completion of the operation, the incision is sutured.
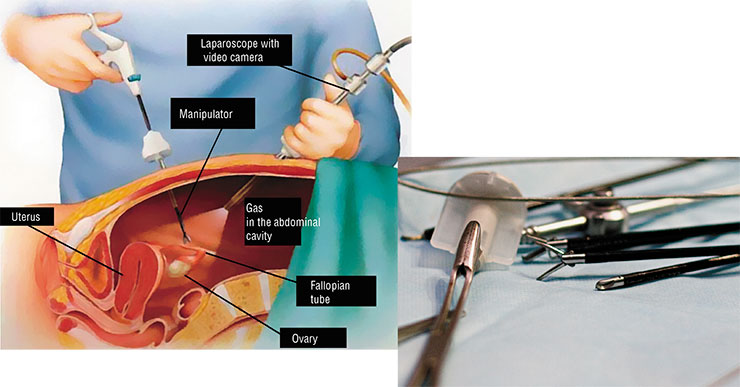
The gallbladder, adrenal, stomach, kidney, ureter, and prostate surgeries can be performed in a similar fashion. In several cases, this sparing intervention provides for performing a combined or simultaneous surgery. For example, a unique operative intervention was performed at the Center for New Medical Technologies in Novosibirsk Akademgorodok: the gallbladder and a calculus from the right ureter of the same patient were removed simultaneously. This operation was performed by two teams of surgeons and took 1 hour and 10 minutes. Two days later, the patient was discharged from the hospital and, in a day, went back to his everyday life.
For women only
The better half of humanity was the first to appreciate the advantages of this new method–by the way, it was a gynecologist who performed the first endoscopic examination.
The state-of-the-art endoscopic methods allow for such complex surgical interventions as a complete or partial resection of the uterus, which is unavoidable when treating some female genital diseases. An ultrasonic Harmonic scalpel made a real breakthrough in gynecological endoscopic surgery. This device is designed according to a two-in-one pattern, i.e., it is intended not only for dissecting tissues, but also for concurrently arresting hemorrhages, which considerably reduces the time required for surgery. Owing to this symbiosis, this tool is very gentle with tissues, and the absence of coarse coagulation crusts enhances a rapid rehabilitation.

Endoscopic intervention is also used to remove various neoplasms of the uterus and uterine appendages. As recently as several years ago, this intervention required a 30 cm long incision in the abdominal wall! This entailed a post-surgery pain and frequent cases of wound suppuration, and looked unsightly. Elaboration of the specialized retractors for laparoscopy has made it possible to remove the neoplasms of practically any size from the abdominal cavity; moreover the resected neoplasm is packaged into a special soft container.
Uterine and vaginal prolapses, accompanied by urinary incontinence and intestinal problems, are among the most acute problems in women’s health. Patients (young women including) with such defects can easily become disabled. The only way out is an operative intervention. These operations have been elaborated long ago, but they are very traumatic. An alternative was designed about 10 years ago–a laparoscopic correction (ventrosuspension) of the uterus, i. e., uterovaginal suspension with the help of a substitute for soft tissues, a mesh tape.
For the heart and joints
All the above described operative interventions are performed within a relatively large space, the abdominal cavity. However, the body has smaller cavities, such as joints or, more precisely, joint capsules. It is very dangerous to enter a joint capsule via a large incision due to the possibility of infectious complications and development of dense intra-articular adhesions after surgery, which can eventually impair the joint function. To avoid this, it is necessary to diminish the traumas of soft tissues within the joint synovial membrane and more gently manipulate with the intra-articular components.
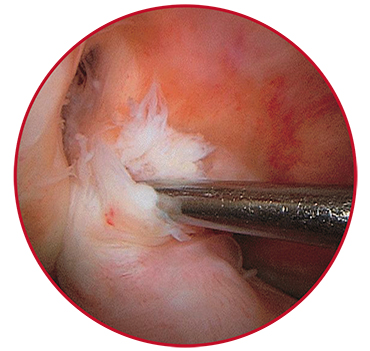 Illustrative in this respect is the endoscopic surgery of the knee joint for meniscus and anterior cruciate ligament tears. In this case, the surgical technique is standard; however, all tools are smaller than these used for abdominal endoscopy. After the intervention, the patients crutch walk for no longer than 10 days and are able to go in for sports without any limitations in about 1–2 months.
Illustrative in this respect is the endoscopic surgery of the knee joint for meniscus and anterior cruciate ligament tears. In this case, the surgical technique is standard; however, all tools are smaller than these used for abdominal endoscopy. After the intervention, the patients crutch walk for no longer than 10 days and are able to go in for sports without any limitations in about 1–2 months.
Recently many people, mostly women, consult with traumatologists and orthopedists about articular pains caused by arthroses of various etiologies. The so-called sanative arthroscopy can be helpful for pronounced degenerative dystrophic joint lesions with bony prominences. In this manipulation, all the altered tissue regions with calcinosis are removed using specialized minute tools and the articular surfaces are smoothed and polished. This makes the life of the patients much easier.
Note that smaller joints can be also affected. Luckily, the surgical endoscopic intervention (to endoprosthesizing) is feasible for joints of any size. Such manipulations have become common for Novosibirsk–they have been performed at the Center for New Medical Technologies for three years.
Arthroscopy is an up-to-date endoscopic procedure for diagnosing and healing the pathologies of joints. For example, when treating the knee joint, an arthroscope is introduced into the articular cavity through a puncture. After examination and determination of the intervention scheme, a pneumatic cuff is put around the thigh to prevent blood accumulation in the articular cavity.In the case of a meniscus tear (which is becoming ever more frequent owing to a rapid development of mountain skiing in this country), only the injured part of the cartilage is resected and drawn outside through the arthroscopic channel.
A complete or partial tear of the anterior cruciate ligament requires a complex surgery, which is also performed endoscopically. The fragments of the ligament are excised, and a new one is constructed out of the ligaments of certain leg muscles (which has practically no effect on the limb function). After a specialized pretreatment of the knee joint, the new ligament is placed and fixed with special resolving polymeric screws and plugs
The endoscopic and minimally invasive procedures have also contributed to cardiovascular surgery. The most well-known manipulation is placing stents, rigid constructs able to preserve their shape, into the coronary arteries, which feed the heart. Mounted on a balloon catheter, stents in a “crimped” state are introduced with an x-ray monitoring into the lumen of an affected coronary artery. When the balloon is inflated, the stent takes the necessary shape, providing a cage for the arterial wall. This method is also used for the diseases of leg arteries.
Another promising minimally invasive surgical procedure has been proposed for improving the myocardial blood supply in the patients after infarction and with severe ischemia. Numerous microscopic holes are made with laser beam in the heart muscle tissue suffering from insufficient blood supply. This enhances blood feeding in the region exposed to laser irradiation; moreover, the development of new arteries around the holes has been observed.
Ice and flame
One third of the world population suffers from varicose veins. Numerous surgical manipulations have been elaborated in attempts to get rid of this malady, which is far from being harmless; however, many of these methods are too traumatic and lead to a high recurrence rate.
A wide use of minimally invasive surgical methods for treating articular and cardiovascular diseases have allowed many patients, including elder people, to come back to an adequate lifeThe basis for minimally invasive intervention for the venous system was established by Galen as long ago as the 2nd century AD; this Roman physician, the founder of modern phytotherapy, also developed a method for destroying varicose veins with special hooks followed by ligation with silk fibers. This approach experienced its second birth in the modern surgical practice. At the beginning of the 20th century, they commenced ablating the affected veins by invaginating and drawing them out with a long flexible probe. However, all these methods were not free of shortcomings, which induced a search for other, more sparing procedures.
One of such methods developed for surgical treatment of varicose veins is the so-called cryostripping–inserting into the vein a special cryosurgical probe with its tip cooled to –85° C. The inner vein walls stick to it, and the vein is removed from its bed. This surgical procedure allows avoiding additional skin incisions and reduces trauma of the soft tissues encompassing the vein, lymphatic vessels, and nerve trunks.

Even more sparing are the methods that stop the blood flow along the vein without its ablation. The scheme for such interventions is similar: electrical current or electromagnetic radiation is applied via a special catheter placed into the vein and causes a thermal degradation of the vein’s inner lining. The catheter is slowly removed from the vein, and its lumen drastically decreases to close completely after a certain time period due to proliferation of the connective tissue.
Recently, the techniques utilizing high energy lasers, whose radiation selectively destroys particular tissues of the venous wall, have been actively introduced. Thus, the subsequent mechanical removal becomes considerably less traumatic.
However, none of the described methods is able to eliminate a cause of varicosis—incompetence of the perforator veins (the horizontal vessels connecting the deep and superficial venous systems). Since 1985, they have started to use endoscopes in the surgery of these vessels, first in Germany and then in other countries. An endoscopic ligature of such veins is now a standard and very efficient manipulation for the patients with trophic venous ulcers, varicose eczema, and pronounced induration of soft tissues.
A medical da Vinci
The achievements surgeons have made thanks to endoscopic methods are impressive. However, medical science is advancing, and the things that seemed fanciful yesterday are becoming an everyday surgical practice. This refers to the transluminal manipulations, implying surgical interventions through the natural orifices without injuring the skin, more precisely, through small punctures in hollow organs (stomach, vagina, gallbladder, and others). The state-of-the-art flexible surgical tools considerably increase the view of the surgical field as compared with a standard laparoscopy. Such surgical procedures are the most painless and least traumatic.
The first transluminal surgical intervention in Russia was performed in February 2008 at the Vishnevsky Institute of Surgery, Russian Academy of Medical Sciences (Moscow). Since June 2008, such surgical procedures have been performed at the Novosibirsk Center for New Medical Technologies.
All the amazing surgical manipulations described above are performed by people, but what would you say about a robot surgeon? Most likely that this is impossible! Nonetheless, such a robot exists and even has a name of its own, da Vinci. It has several skillful limbs able to make very precise movements; various trocars with the necessary surgical pieces can be attached to the limbs.

The design of da Vinci surgical system is based on the structure of human wrist: the cables in manipulators play the role of tendons. Monitoring the process using a video system, a surgeon outside the operating room can remotely control the robot with the help of special joysticks.
The camera-based control system has a manual control unit and the foot switches to move the camera closer or farther from the objects and even rotate it. If necessary, the image of the surgery site can be magnified up to 12-fold as compared with its real size.
It is the video system that makes robot-assisted surgery so attractive to surgeons. Specialists who have an experience of such interventions say that it feels as if they were present at the operation and worked themselves with “minute hands” inside the patient’s body.
We can only fantasize about the future achievements of medical science, including surgery: in many ways, they will depend on advances in the rapidly developing scientific fields. The issues which presently seem topical and promising can turn a dead end, whereas the things presumptuously rejected or looked upon as unreal, on the contrary, could resolve most intricate problems in medicine.
References
Minimally Invasive Surgery: A Manual for Physicians / A. S. Bronshtein, ed. Moscow: MIPI, 1995.
Minimally Invasive Surgery: Internet Journal (www.laparoscopy.ru/review). No. 3 (8). March 15, 2004.
Khasanov, A. The Access is Simple and Genial: with the Help of New Flexible Endoscopes, Surgery Rises to a New Developmental Stage // Meditsinskaya gazeta. 2008. N. 14. P. 10–11.
The photos are by the courtesy of E. Platova (from the archive of the Center for New Medical Technologies, Institute of Chemical Biology and Fundamental Medicine)











