Chronic Lyme disease: nonexistent illness or wrong diagnosis?
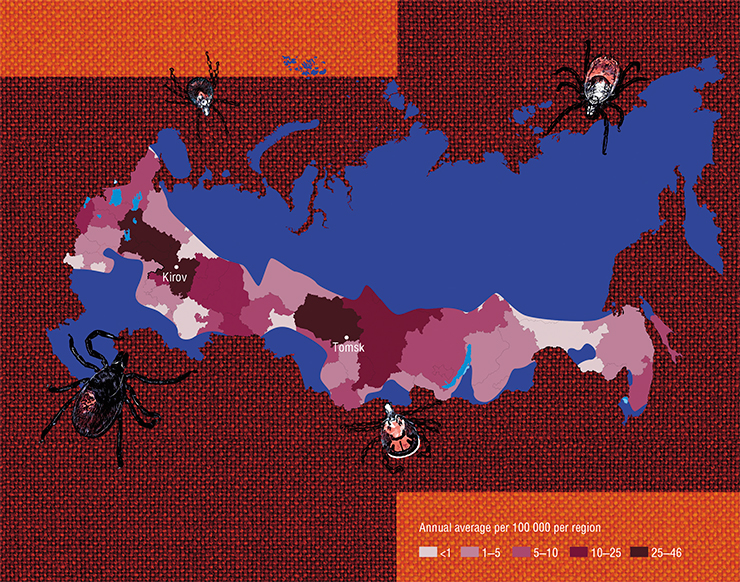
Every year thousands of people worldwide, primarily in Russia and the United States, contract a disease called tick-borne borreliosis (Lyme disease). In 2017, around 60 thousand cases of tick-borne infections were registered in the US alone; in 82% of the cases, it was Lyme disease. However, some estimates predict the real number of people infected with Lyme disease annually could be greater by an order. In the majority of cases, patients are successfully treated and cured with antibiotics, however, in 10 to 20 percent of all patients the disease develops into a serious chronic form. Experts still do not know why this happens. The difficulty of diagnosing tick-borne borreliosis and the broad range of its symptoms often complicate correct diagnosis and timely prescription of treatment in patients seeking medical help
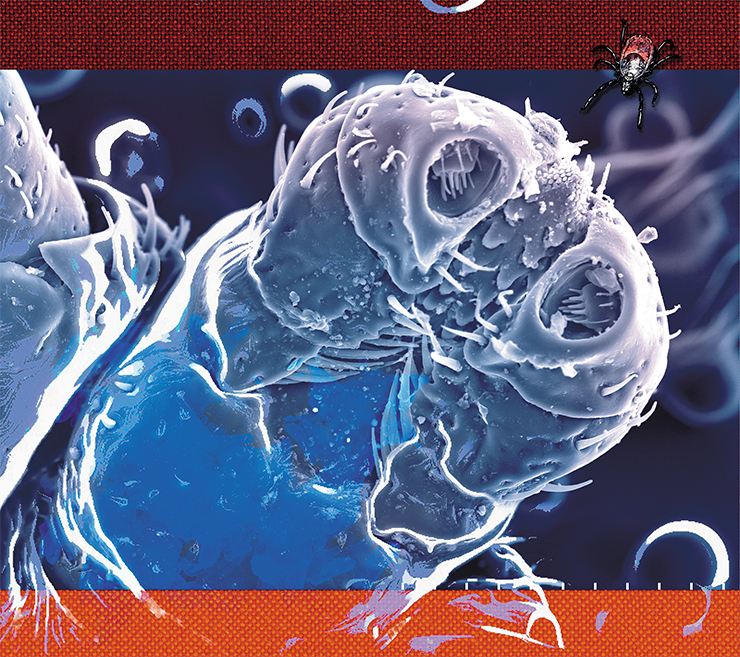
Tick-borne borreliosis, or Lyme disease, is a tick-transmitted polysystemic infections disorder with a wide range of manifestations: cutaneous, arthral, neurological, cardiological, etc. The first symptoms appear within several days or weeks after the tick bite; late-onset symptoms can emerge months and years after infection. Both the symptoms and the course of the disease differ greatly from patient to patient.
A peculiar red swelling in the form of extending concentric rings may appear at the point of the bite of an infected tick and spread across the body surface. This is the so-called migrating erythema – a dramatic evidence of the proliferation and spread of the infectious agent – Spirochete bacteria. However, the peculiar reddening does not develop in all infected patients, and the absence of erythema does not mean a lesser risk of the development of Lyme disease in a person bitten by a tick. About 30–40 % of such patients never even noticed the tick bite that caused the disease.

Anyway, a definitive clinical diagnosis in many cases is impossible without laboratory confirmation. However, some of the enzyme immunoassay tests used nowadays are imperfect. The standard enzyme immunoassay, instead of Borrelia themselves, registers antibodies produced by the organism in its fight with these bacteria; these antibodies can be detected only after 3–4 weeks of infection. For this reason, such test often produce false negative results, especially in patients whose immune system failed to produce an adequate immune response. These test systems are known to produce false positive results, too. There are more laborious methods based on detecting a number of bacterial proteins, but they are never completely accurate, either.
NO VACCINE YET Despite all efforts, attempts to develop an efficient human vaccine against tick-borne borreliosis have failed (Embers, Narasimhan, 2013).Initially, researchers suggested to use surface proteins of the infectious agent for the vaccine; these proteins were studied thoroughly to reveal the most promising immunogens. The “winner” was a surface protein called OspA, which was found to cause the strongest immune response and became the basis of LYMErix, which was produced by the American company SmithKline Beecham. However, the production was stopped after serious side effects were reported. It was found that the antigenic properties of OspA were similar to a human protein important for the functioning of lymphocytes, and in some cases, vaccination caused autoimmune disorders.
Researchers were forced to follow an unorthodox path, trying to develop vaccines capable of suppressing the very process of infecting of humans by ticks. For instance, such vaccine can be aimed at proteins of the tick saliva, disrupting the latching and feeding process of the parasite.
For the past 20 years in veterinary medicine, traditional vaccines made of bacteria inactivated with formalin have been used. Recently, more advanced vaccines based on the OspA and OspC proteins appeared. Their efficacy has been proven on dogs; however, our knowledge about their safety and side effects is incomplete
Therefore, laboratory tests may confirm the diagnosis, but negative test results cannot be considered as a proof of absence of Lyme disease. The doctor must analyze the whole picture of the illness in a particular patient. This is not easy, since the symptoms of the involvement of the brain in the pathologic process of Lyme disease are similar to those of a number of neurodegenerative disorders; meanwhile, such symptoms as fatigue and headache can accompany all sorts of diseases, and not only infectious diseases.
Patients with normally functioning immune systems are thought to produce active immune response to the invading Borrelia, in a way that the bacteria may be wiped out even without the standard therapy. For Lyme disease, antibiotics are used, with the best results produced by ceftriaxone and doxycycline. Modern medicine prescribes prophylactic use of antibiotics for patients with high risk of infection (those bitten by a tick or exhibiting migrating erythema, etc.) and a two or three week-long course of antibiotics if the disease develops.
Despite all these measures, the disease turns chronic in some patients, when even repeated courses of antibiotics fail. Here, the situation is complicated by the difficulty in establishing the reasons underlying this condition. The lack of knowledge about mechanisms of damage caused by Borrelia infection, drug resistance, and the unreliability of modern methods of clinical diagnostics has spawned numerous opposing views on this problem.
Disease or syndrome?
The problem of tick-borne borreliosis is disputed among doctors and scientists as well.
According to an opinion, standard therapy with antibiotics fails to destroy the infectious agent completely in patients with compromised immune systems. This opinion is confirmed by experiments on laboratory animals: weak Borrelia were found after treatment with antibiotics in infected laboratory mice and primates. Some research results tell that Borrelia possibly persist organs and tissues as biofilms – colonies of microorganisms embedded into a polymer matrix that they produce. In this form, Borrelia become virtually unreachable to drugs and immune cells.
Symptoms of late stages of the disease are highly variable. Some patients experience disruptions of the heart rhythm, inflammation of the eyes and liver, and extreme fatigue. Neurological complications include severe depression, memory impairment, insomnia, frequent headaches, intolerance to light and sounds, hallucinations, encephalomyelitis, etc
According to another view, no live Borrelia remain in the body after a course of antibiotics. However, in the course of the disease, the bacteria disrupt the normal work of the immune system, which later manifest in autoimmune disorders for extended periods. For instance, some peptidoglycans of the bacterial cell wall are strong immunogens and can persist in the body for a long time. Long-term toxic effects can also be caused by the remains of biofilms with dead Borrelia. All these bacterial components provoke inflammation that affects various organs and tissues, causing such problems as arthritis. This condition has been named post-Lyme syndrome (Blaut-Jurkowska, Jurkowski, 2016).
Incidentally, a number of experts believe that chronic Lyme disease develops in cases when the patient is simultaneously affected by Borrelia and other tick-born infectious agents, such as Ricketsia. Very often, ticks carry several infectious agents, and some of them cause symptoms that are very difficult to distinguish clinically.
Crossing swords
The issue of chronic borreliosis is especially acute in the USA, where, until recently, the Infectious Diseases Society of America (IDSA) denied its very existence. Only in 2019, it was officially acknowledged that a number of non-specific symptoms can persist in some patients for a long time after the treatment of Lyme disease. However, without clinical proof of the presence of live Borrelia in the patient, IDSA does not recommend to associate such symptoms directly to the disease or appoint additional courses of antibiotics. Consequently, insurance companies refuse to pay for treatment of these patients, who suffer from a “nonexistent” disease.
CURE AS IF BY MAGIC The problem of chronic borreliosis in the USA is complicated by the activities of various “healers” and “experts on chronic Lyme disease”, who are whipping up public fears and prey on their patients. They scare patients who experience ailments of different nature, unconfirmed by a definitive diagnosis, into believing that they have chronic Lyme disease, and prescribe expensive treatment following their own “schemes”, even though extended, months-long antibiotics therapy can be detrimental to the weakened organism. Moreover, by wasting time on quacks, patients fail to receive proper treatment for their real diseases, such as Alzheimer’s. Ultimately, such patients come back to real medical professionals, having lost thousands of dollars and countless hours on useless procedures.In Russia, the situation with chronic borreliosis and complications following the disease is rather similar, with the same unreliable diagnostics and scientifically unfounded recommendations regarding the prophylaxis and therapy of the disease. Apparently, there are many patients suffering from chronic infection, which has not been diagnosed and treated in time. There are hordes of quacks offering cures for any disease – as long as you pay. To make it worse, there are representatives of the conventional medicine establishment who attempt to treat diseases such as tick-borne encephalitis with homeopathy and various concoctions without efficacy proofs or proper clinical trials, such as iodantipyrine (Russian йодантипирин, an iodine-containing pyrazole derivative claimed to have antiviral properties). Some even use placebo drugs without active compounds, such as Anaferon (Russian Анаферон, produced by a company called Materia Medica Holding (sic!) headed by O. Epstein, notorious for being in the limelight of a recent investigation by the Commission on Pseudoscience and Research Fraud of the Russian Academy of Sciences)
Thousands of people across the US disagree with this position, as they have been suffering from serious disorders that they believe are associated with consequences of tick-borne infections. Chronic Lyme disease was first recorded in the USA 45 years ago: according to some estimates, there are up to 400 thousand patients suffering from the disease. These people, together with some medical professionals founded the International Lyme and Associated Diseases Society (ILADS), which promotes aggressive antibiotics therapy in cases when the observed symptoms are suspected to be caused by a Borrelia infection.
Proponents of the official view believe that the chronic Lyme itself is a creation of dishonest doctors exploiting the dire situation of their patients with poorly determined diagnoses. In their opinion, instead of additional antibacterial treatment, patients in whom modern diagnostic methods fail to detect Borrelia infection need psychiatric help. As the result, people who consider themselves chronically infected are forced to turn to doctors who disagree with the official position, and cover treatment costs from their own pocket.
However, the majority of doctors in the US and Canada adhere to recommendations of the official medicine, which has sparked up true “Lyme wars”. Some experts state that Lyme disease research has become so badly entangled with politics that it creates problems with publishing works on chronic borreliosis in American medical journals and in funding research aimed at the study of this disease.
The truth is somewhere in the middle?
 Is there such thing as right and wrong in these Lyme wars? The reality seems to be way more complex.
Is there such thing as right and wrong in these Lyme wars? The reality seems to be way more complex.
For instance, there is recent experimental proof that patients with post-Lyme syndrome suffer not just from some psychological problems, but rather, from very specific brain lesions. Their blood, as well as eight of the brain’s regions, have been found to contain elevated amounts of a protein known to be a marker of inflammation. In the six months after the course of antibiotics, these patients experienced extreme fatigue, lack of concentration, and impairment of memory and cognitive functions (“brain fog”) (Coughlin, Yang, Rebman et al., 2018). Due to inflammatory processes and lesions caused by Borrelia infection, such neurological symptoms can persist for weeks and months even after a long initial course of antibiotics.
The question is, whether live Borrelia remain in the body? In the majority of cases, even extended courses of antibiotics failed to relieve the suffering in patients with the chronic form. That means that most often, the answer is “no”. In addition, such courses of antibiotics themselves can be detrimental to the patients’ health by destroying the normal bacterial microflora of the intestine, causing allergic reactions and other negative effects.
However, in some rare cases of chronic borreliosis, additional antibiotic therapy turned out to be efficient. It is possible that in some patients, live Borrelia indeed remain after a standard, untimely, or incomplete course of treatment, meaning a true chronic illness. Remember that laboratory diagnostics of Lyme disease nowadays is unreliable. Moreover, in chronic borreliosis, the infections agents can be contained primarily within neurons, i. e. beyond the blood-brain barrier. Diagnostic systems have low sensitivity and cannot be used for patients with low bacterial titer in the blood.
Therefore, everything depends on the specific situation. In some cases, we deal with true chronic infections, while in other cases it is post-Lyme syndrome, which develops after the illness.
Biosensor for the tick and PCR for humans
One of the main problems with Lyme disease deals with diagnostics at early stages of the disease. The earlier you begin the treatment, the higher the chance of avoiding the disease becoming chronic.
Nowadays, there is a direct method of detecting Borrelia in blood at early stages of infection. It is known as PCR-diagnostics, where bacterial DNA is detected using polymerase chain reaction. However, simple variants of this method are not sensitive enough, while highly sensitive methods, based on a combination of PCR with mass-spectrometry, are too complicated and expensive for clinical use. Recently, an American company, Ceres Nanosciences, developed a new direct method for detecting Borrelia in the body. It employs special nanoparticles, which trap bacterial antigen molecules from large volumes of the patient’s urine. Once concentrated in this manner, these antigens can be detected with conventional immune analysis (Magni, Espina, Shah et al., 2015).
A team of students from the M. V. Lomonosov Moscow State University together with experts from the V. A. Engelgardt Institute of Molecular Biology (Moscow) and other research institutions began the development of a method of express diagnostics of Borrelia infection of the vector itself – the ixodid tick.
LYME DISEASE AS CAUSE OF NEURODEGENERATIVE DISORDERS? A group of American researchers suggested a hypothesis about a possible connection beween Lyme disease and the development of neurodegenerative disorders. They were prompted by the similarity of symptoms observed during late stages of Lyme disease and symptoms typical for Alzheimers’, Parkinson’s and even autism (MacDonald, 2006; Miklossy, 2008, 2015). The hypothesis is supported by the fact that Borrelia, like its close relative, Treponema, the infections agent of syphilis, can enter the brain and cause lesions characterized as neuroborreliosis (Lapenta, 2018).Indeed, Borrelia bacteria have been found in thin sections of brains of patients who died of neurodegenerative disorders. The authors believe that Borrelia biofilms were located within amyloid plaques similar to those observed in patients with Alzheimer’s (Miklossy, 2016). They speculate that the immune response to these biofilms is what causes Alzheimers’, and that the person may have been infected with Treponema or Borrelia long before their brain was affected. However, no definitive proofs of this hypothesis were found.
Research in the National Institute of Health failed to detect Lyme disease markers in such patients. The main argument against this hypothesis was the analysis of distribution of these diseases across the US, since Lyme disease, unlike the neurodegenerative disorders in question, only occurs in several states on the East Coast (Forrester, Kugeler, Perea et al., 2015). The researchers failed to acquire any definitive data supporting the connection of Lyme disease with neurodegenerative disorders
Currently, the tick to be analyzed is removed from the body and brought to a specialized laboratory, where the infectious agent is detected using PCR or enzyme-linked immunoassay. The analysis takes several hours and is only possible in laboratory environment. The new biosensor is based on detecting borrelia DNA in the sample using genetically engineered molecular structures created based on a system constructed from components of the well-known molecular complex for genome editing, CRISPR/Cas.
This binary system contains two RNA molecules complementary to two adjacent sequences in the bacterial DNA. These RNA carry two proteins, which are compounds of an enzyme called beta-lactase. If the examined sample contains Borrelia DNA, the RNA binds to it, and their protein subunits joins, forming an enzymatically active complex that results in the synthesis of a certain dye in the presence of a specific substrate. The change of color of the solution can be registered using a simple portable spectrophotometer.
Today, the situation with chronic Lyme disease remains distressing. There are too many unanswered questions dealing with diagnostics and therapy recommendations for patients who have this tick-borne infection.
One of the most controversial issues is whether to hurry with antibiotics after the tick bite. There is an official recommendation stating that if the tick has latched for less than 24 hours, there is virtually no danger of infection. The problem is, people with Lyme disease often do not remember the bite as the disease can be transmitted by tiny tick nymphs, whose bite can go unnoticed, and by males, who only latch for a short time. At the same time, the majority of physicians in the US and Europe believe that the lack of characteristic symptoms in the days following infection means there is no need for antibiotics. This position is difficult to agree with, keeping in mind that the development of the infection can result in long-term disruptions in the normal function of many systems of the organism.

We can answer all these questions only when researchers get to the grips with the tricky secrets of these treacherous bacteria. Until then, quacks will continue to rob their patients and insurance companies will keep wiggling out of payments. However, adequate large-scale study of tick-borne infections and the development of efficient diagnostics and treatment measures require sufficient funding.
In the US, patients themselves have joined efforts to change the situation with funding the study on Lyme disease through the Congress. A similar movement once emerged in the wake of the AIDS epidemic, resulting in efficient measures on the organization of intensive HIV research. Today, this illness is no longer a death sentence. If similar efforts are applied to the study of tick-borne borreliosis, very this disease can not pose such a threat to our health as it does now.
References
Blaut-Jurkowska J., Jurkowski M. Post-Lyme disease syndrome // Pol Merkur Lekarski. 2016. V. 40(236). P. 129–133.
Coughlin J. M., Yang T., Rebman A. W. et al. Imaging glial activation in patients with post-treatment Lyme dis-ease symptoms: a pilot study using [11C]DPA-713 PET // Journal of Neuroinflammation. 2018. V. 15(1). DOI: 10.1186/s12974-018-1381-4.
Embers M. E., Narasimhan S. Vaccination against Lyme disease: past, present, and future // Frontiers in Cellular and Infection Microbology. 2013. V. 3(6). DOI: 10.3389/fcimb.2013.00006
Forrester J. D., Kugeler K. J., Perea A. E. et al. Geographic Correlation between Lyme Disease and Death Due to 4 Neurodegenerative Disorders, United States, 2001–2010 //Emerg Infect Dis. 2015. V. 21(11). P. 2036–2039.
Fomenko N. V. Tick-Borne Borreliosis: A Life-Long Disease? // SCIENCE First Hand. 2007. V. 15. N. 3. P. 44–51.
Lapenta J. M. Lyme Disease and Dementia, Alzheimer, Parkinson, Autism, an Easy Way to Destroy your Brain //Investigative Dermatology and Venereology Research. 2018. V. 4. N. 1. P. 30–43.
Livanova N. N. Octopod Vampires // SCIENCE First Hand. 2006. V. 11. N. 6. P. 80–83.
Miklossy J. Historic evidence to support a causal relationship between spirochetal infections and Alzheimer’s disease // Front Aging Neurosci. 2015. V. 7(46).












