Spare Parts for the Human Body
What can possibly be in common between fancy cookies, the blade of and ice ax and a metal implant? Surprisingly, all of them can be made using the same technology or, more precisely, the same family of modern technologies. In technical literature, these technologies of “3D-printing”, or “free sculpturing” of the complex volume shapes are often referred to as Rapid Prototyping. Today the more general and precise term, “additive manufacturing”, is becoming increasingly common. Additive manufacturing technologies (AM) are applicable to very different materials – from food (dough, chocolate, cheese) to polymers and hard metal alloys. Today these technologies are finding new applications in medicine and biomedicine – in particular, in the manufacturing of individually fit implants
The human body continues to surprise us. Despite its seemingly fragile constitution as compared to the inanimate matter, it consists of rather tough “parts,” capable of withstanding strong external and internal forces. There are certain limits though, and for centuries in legends and fairy tales we have been dreaming of Golem, Tin Man, robots and the Terminator, where the “weak human flesh” is substituted by stone, metals, ceramic and polymers.
THE COST OF A PROTOTYPEIn order to reduce the potential costs of potential failures, computer-aided design together with the finite element modeling of the components and assemblies is used at the early stages and prototyping at the final stages of the design.
Large size prototypes are often hand-crafted using gypsum, clay, wood or foamed plastic. For the smaller size objects, computer-guided “3D printing” presents a versatile, fast and cost-effective alternative
Beginning from the end of the 20th century, the dream of substituting the damaged, traumatized and ageing body parts has started to become a reality thanks to the advances in multiple areas of modern science and technology, from biology and psychology to technical design and manufacturing.
Freedom of shape
Modern industrial technologies of additive manufacturing utilizing the latest advances in the material sciences and information technology, when consecutive layers of material are added to a component, received their name in contrast to the classical cutting ones, when the excess of material is removed from the bulk piece. Additive manufacturing methods are very effective in the manufacturing of components with complex shapes, which is reflected in the corresponding Swedish term ‘friforms-teknologi’, or the technology with the freedom of the shapes.

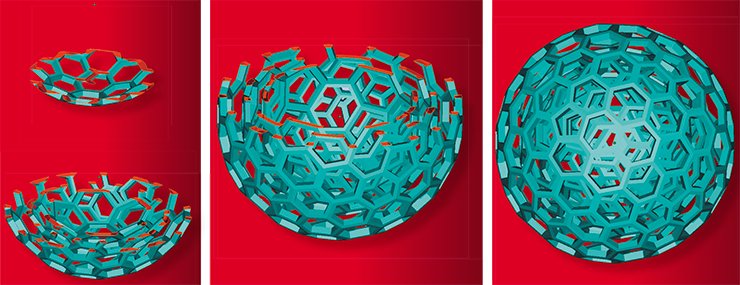
Additive manufacturing starts within the modern software of computer aided design (CAD). Because AM technologies are based on adding the working material in consecutive layers, corresponding 3-dimensional CAD drawing must be “sliced” generating separate “flat” drawings for each of the working layers. Each of these 2-D drawings contains the information where the working and support materials should be placed during manufacturing. A prepared file with the ‘slices’ and additional processing information is sent to the AM machine that can be regarded as a “3-D printer.”
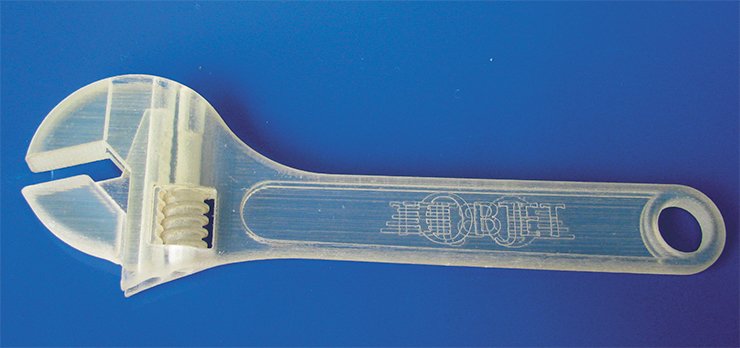
Additive manufacturing devices use a few different principles of operation. The ones working with polymers may use fine granules of polymer molten by laser (e. g. Selective Laser Sintering, or SLS), or work similar to the true jet printers using polymerizing liquid chemicals, or extrude the thermoplastic material through a thin nozzle, like in the FDM machines. However, all AM machines construct the components placing thin layers of the working material one over another thus “printing” in three dimensions.
For example, the working head of PRODIGY plus FDM machine, a distant relative of the common glue gun, moves under computer control in the horizontal plane and squeezes a thin wire of molten polymer placing it over the previous layer of hardened plastic. After finishing work over the current layer, the machine moves the start platform one step down. A high temperature is kept in the working chamber to provide good adhesion of the consecutive layers. And so, layer by layer, the component grows up taking its shape.
In 48 hours
When engineers talk about the “limits of the body constructions,” this is first of all related to its “rigid frame,” the skeleton. Human bones are capable of sustaining significant static and dynamic loads, at the same time providing certain flexibility of the body through numerous joints. However, when the strength limit of the bones is exceeded, they break.
Usually, to mend the broken bones, it is enough to put them together and immobilize them with the plaster of Paris for a few weeks. In other cases, a surgery is needed. Sometimes the elements of our “rigid frame” are damaged to such an extent that they need partial or full replacement. One of the largest problems in the medical and biomedical implant manufacturing derives from the ultimate diversity of the shapes and sizes of the implants needed, from relatively simple bone fragment fixation plates to very complex ones designed to replace large sections of bones or even complete joints. The dimensions of even similar human bones are highly individual for each person, thus even in the relatively simple surgical cases it is often needed to adjust the shapes and dimensions of the standardized “orthopedic Mechano-kit” during the operation. Thus an operation theatre is becoming a mechanical workshop, with the surgeon cutting and bending metal pieces for better fit while the patient is under full anesthetic.
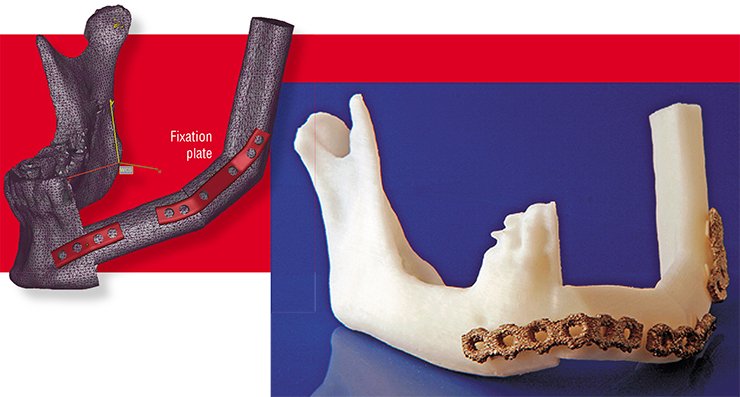
The situation is even more complicated with more complex implants. In industry there is a common way of lowering the manufacturing costs and bringing products from the “unique” to the “affordable” category. This is achieved though bulk production of the same component, identical in shape and size. However, there is no such “one-for-all” implant, and manufacturing of the “unique-for-each” ones using traditional technologies in many cases is prohibitively expensive.
Today manufacturing of a limited number of the implants with fixed shapes and sizes helps to keep the balance of the implant costs. In many cases there are only ten-twelve standard sizes of the same type implants certified and used in surgery. As a consequence, the surgeon is often forced either to remove some parts of the patient’s bones or to fill the gaps with the “bone cement” to better fit and fix the chosen implant.
It is said that a good surgeon “thinks wit his hands.” Indeed, many surgeons prefer to plan the operation not in front of the computer screen, but using the real models of the bones. Traditionally such models are made out of gypsum or plastic by an artist, basing upon the X-ray images or CT scans. This process is laborious and lengthy, and in many cases the operations cannot be postponed.

Today additive manufacturing technologies can be efficiently used not only to manufacture the anatomically precise pre-operative bone models, but also the tools for helping surgeons during the operation, for example the plates for precision guiding of the saws and drills.
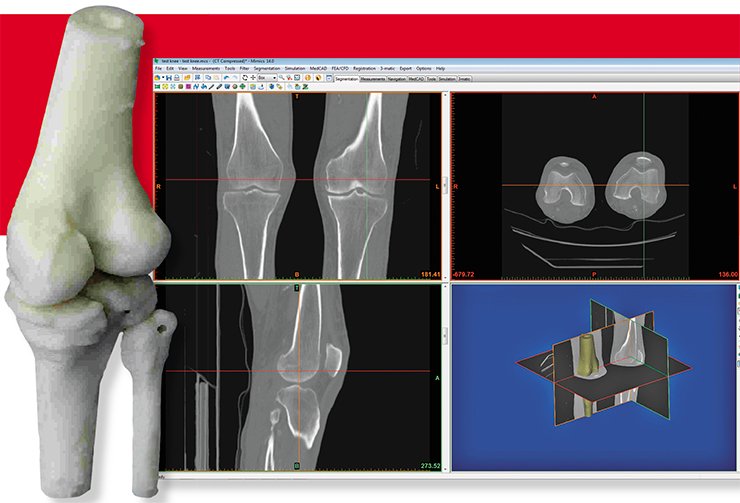
Preparation of the data starts from the computer filtering of the medical image (most commonly, X-ray or CT image). The result is a precise three-dimensional computer model of the human body, including soft tissues, cartilage and bones. After that, this image is “filtered” using special software to generate a precise 3-D image of the bones alone.
 As the original images have extremely high spatial resolution, models constructed directly from them are very complex and being transferred as they are into the engineering software packages demand extreme computational resources for further processing. Therefore, the models are simplified: all surfaces are represented by a large number of simple flat polygons (such representation is quite common for many design and engineering software packages). At this stage the models can be efficiently handled by the software that can, for example, compute the mechanical properties of the bones or prepare the files for the 3-D printer that can make bone models from the polymer.
As the original images have extremely high spatial resolution, models constructed directly from them are very complex and being transferred as they are into the engineering software packages demand extreme computational resources for further processing. Therefore, the models are simplified: all surfaces are represented by a large number of simple flat polygons (such representation is quite common for many design and engineering software packages). At this stage the models can be efficiently handled by the software that can, for example, compute the mechanical properties of the bones or prepare the files for the 3-D printer that can make bone models from the polymer.
The time needed for the file preparation until it can be sent to the additive manufacturing machine depends on the complexity of the part but as a rule it does not exceed one full day. It takes about one more day to manufacture the plastic bone model. Thus in two day’s time a surgeon will be able to get a precise pre-operative model.
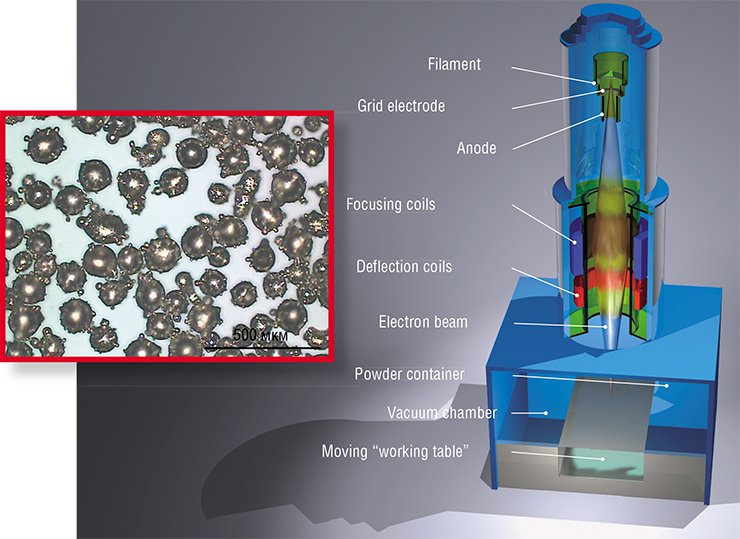
Alloys certified for medical applications melt at high temperatures (titanium-aluminum-vanadium alloy, for example, has a melting temperature about 1650 °C) and extruding them through the nozzle is hardly possible. Instead of that, additive manufacturing machines use computer-guided melting of the thin layers of fine working powder by a high energy laser or an electron beam.
Alloys for medical and biomedical applications are quite special: they must be strong, durable, non-corrosive and biocompatible, e. g. they should not cause any adverse reaction when placed inside the human body. Electron beam melting machines routinely use titanium-aluminum-vanadium (Ti-Al-V) and cobalt-chrome alloys allowed for implant applications in the EU and USA. It commonly takes a few days from receiving the medical imaging data until an individually fit implant can be delivered for a surgery, nearly the same time it needs to prepare a complex surgery. There is an additional bonus: the EBM- implants are perfectly sterilized during the manufacturing process, which takes place in high vacuum at very high temperatures.
Following the path of Nature
With all its advantages, the manufacturing of perfectly fit individual implants solves only one of the problems existing in orthopedics. The implants substituting “damaged parts” should be operating inside the human body, and the task of their perfect functionality and long-term operation without failures has not been solved yet.


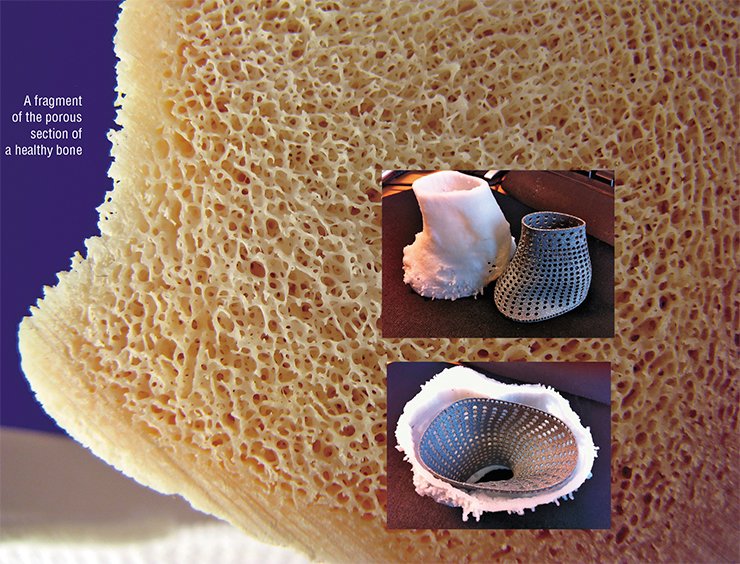
One should note that our bones, even these we assume to be solid, have quite a complex structure including solid, meshed and porous sections. But a dominating majority of modern implants are made of solid metal, preventing normal transport of biochemical fluids in the areas adjacent to their surface and thus slowing the process of their integration with the new growing bone.
 Also the solid metal implants are much stronger than the bones they are designed to substitute: titanium rod a little thicker than an ordinary pencil is capable to withstand loads equivalent to a heavy truck running over it. None of the human bones can have such load capacity. Such unbalanced properties often facilitate secondary bone fractures near the implant, where the bone is not protected by the metal.
Also the solid metal implants are much stronger than the bones they are designed to substitute: titanium rod a little thicker than an ordinary pencil is capable to withstand loads equivalent to a heavy truck running over it. None of the human bones can have such load capacity. Such unbalanced properties often facilitate secondary bone fractures near the implant, where the bone is not protected by the metal.
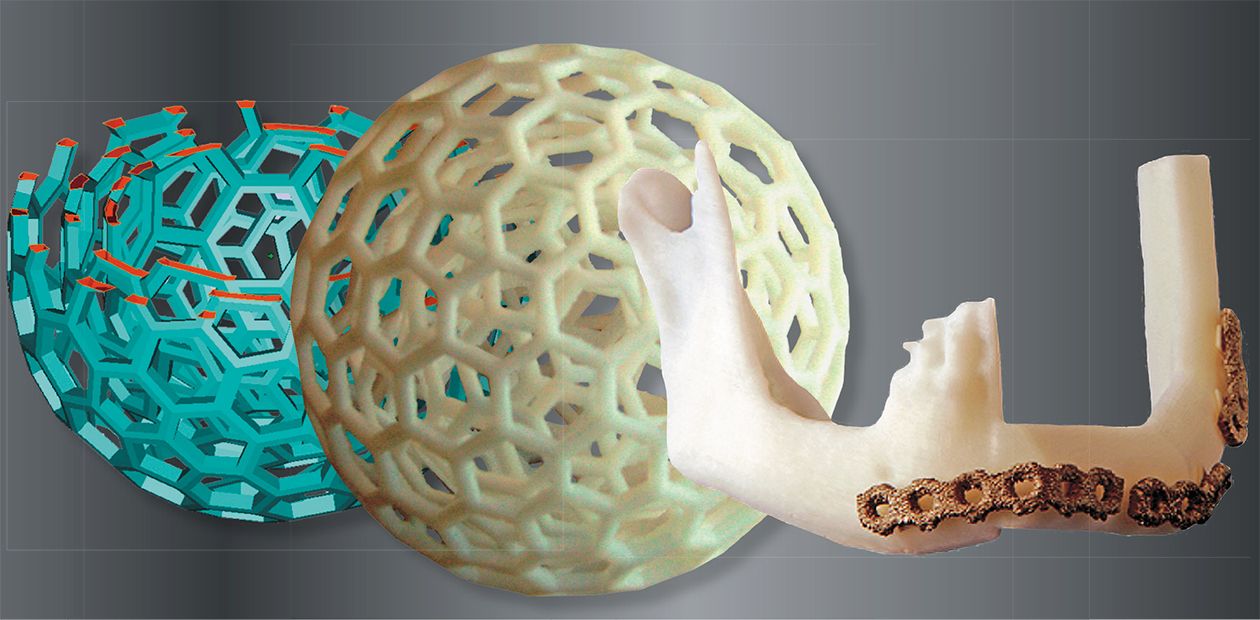
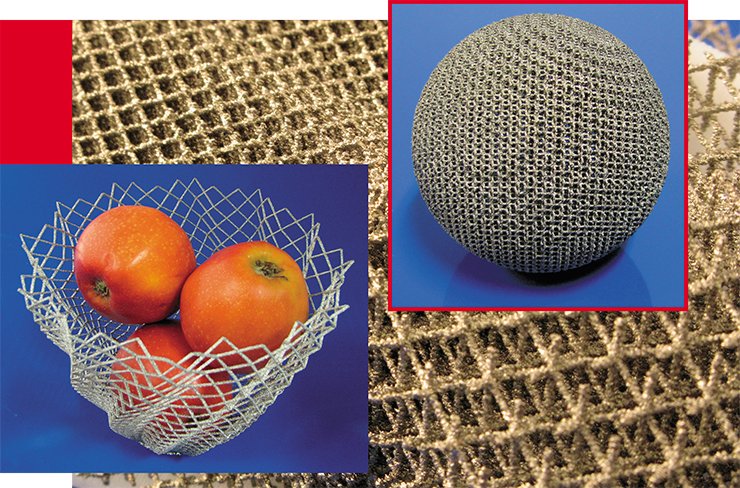
It means that not only the shape but also the structure of a metal implant should mimick the human bones, this including solid, mesh and porous sections. Using traditional ways of manufacturing, it is almost impossible to make the structures with integrated solid and meshed sections. Additive manufacturing technologies can achieve this in the same manufacturing process.
New growing bones penetrate into the light 3-dimensional mesh structure integrated with the solid part of the implant. Such reinforced interface between the natural bone and the metal of implant is much stronger than in other cases.
As mentioned above, the excess strength of the metal structures substituting natural bones could present a problem. It can be solved by replacing solid metal structures with the ones with a solid metal core and a variable density mesh in the outer parts. Varying the geometry of such structures, it is possible to adjust their mechanical properties to the ones of the replaced human bones. So the outline of the outer mesh will perfectly fit the surface of the bone and the inner solid core will provide the implant rigidity.
It is also known that a newly growing bone adheres better to the rougher implant surfaces. Therefore, the traditionally manufactured metal implant surfaces interfacing the bone are additionally roughened. In EBM technology the surface mesh-type and rough surfaces are achieved within the same manufacturing process.
The design of the outlines and structure of the implants today is carried out by the engineering programs that can also calculate the weight, rigidity and other mechanical properties of the construction. Thus it is possible not only to design the implants ideally following the geometry of the bones but mimicking their mechanical properties. In other words, it is possible not only to design a perfectly fitting implant but also the one with a desired functional behavior. For example, it is possible to design hip implants having maximum mechanical strength near the joint and fitting geometry and mechanical properties of the natural bone in the stem part.
Surface matters
The strength and long-term stability of the bone attachment to the implant depends not only on the chemical composition of the implant bulk and surface, but also on the surface micro-geometry. It is understandable, as implanted materials are becoming involved into the processes going in the human body at both the cell and biochemical levels. Thus an ability to correctly adjust the properties of the implant surface is quite important.
According to some of the existing data, advantageous conditions for the osteoblast (cells initiating the new bone growth) fixation are provided by the surface with the roughness corresponding to the surface features of about 40 µm (for comparison: the thickness of a human hair is about 10—100 µm). It may also appear that the optimum surface roughness is much smaller, with the features much less than the size of the cells.
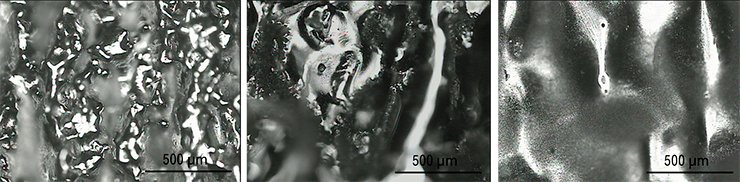
Additive manufacturing technologies are easily capable of controlling the geometry features from tens centimeters down to fractions of millimeters, e.g. about the thickness of the working powder layer (with ARCAM EBM machine the layer thickness today is 0.07 mm). But as we have pointed out earlier, in many cases surface control down to micro- and nanometer scale is needed

The untreated surfaces of the components manufactured in the EBM machine may have certain amount of partly fused powder grains. There is always some risk that being placed in the human body such grains can leave the implant surface.
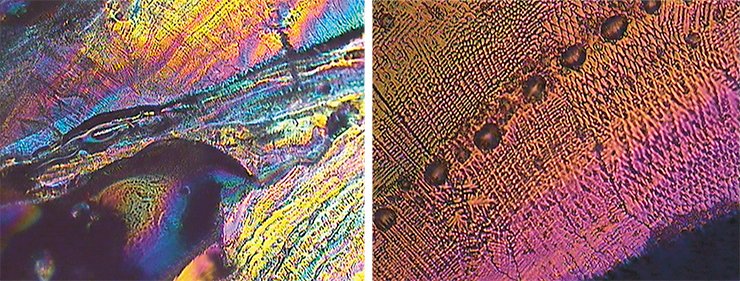
Today the most promising technologies for the surface post-processing of the implants manufactured using the AM technologies are regarded to be plasma etching (in vacuum or low pressure gas atmosphere) and chemical and electrochemical etching (in solutions). Electrochemical etching helps to remove the potentially loose powder grains from the surface and to “polish out” small elements of the surface micro-landscape.
Attachment of the bones to the implant also assumes some chemical bonding with the implant surface. Thus changing the chemical composition of the implant surface it is possible to facilitate better bone attachment to the implant.
Chemical and electrochemical methods are also capable of an implant surface modification. For example, it is possible to oxidize the surface of implants, or to cover it with the bioactive compositions such as hydroxyapatite, one of the calcium phosphate crystal forms present in natural bone material.
Some years ago the emerging computer assisted design technologies have revolutionized the design process. Because of them it became possible to coordinate the work of multiple designers often located in different parts of the world, to easily modify and model the properties of the components – in the virtual world. Together with additive manufacturing these methods result in unprecedented capabilities of the fast materialization of the designer’s ideas.
Using two of these modern technologies together one can not only perform virtual surgery again and again, optimizing the procedures before it is done “for real,” but also to manufacture the plastic bone models, metal implants and fixation plates, and optimized tools for the future operation.
These technologies have not yet become a routine. But most technological aspects of the manufacturing of “spare parts” for the human body have already been successfully resolved. We hope that in the near future additive manufacturing technologies together with other methods of modern engineering can satisfy the demands for the individually fit implants, optimized for both mechanical properties and functionality.
References
Cronskr M., Rnnar L.-E., Bckstr m M. Implementation of Digital Design and Solid Free-Form Fabrication for Customization of Implants in Trauma Orthopaedics // Journal of Medical and Biological Engineering. 2012. V. 32. № 2. P. 91—96.
Koptyug A. et al. Electron Beam Melting: Moving from Macro- to Micro- and Nanoscale // Proceedings of the Intl. Conference on Processing and Manufacturing of Advanced Materials, THERMEC-2011. Quebec, Canada, August 1—5, 2011.
Cronsk r Met al. Application of electron beam melting to titanium hip stem implants // Proceedings of Intl. Conference on Additive Technologies, September 17—18. Ptuj, Slovenia, 2008.
The photographs are from the archive of the Additive Manufacturing Group of the Institute of Engineering and Sustainable Development, Mid Sweden University (Östersund); and courtesy of Dr. Per Dérand (Lund University) and Prof. Jan Hirsch (Uppsala University Hospital)